Improving Hamstring Flexibility - part 1 Assessment.
Introduction
In recent years, research has been conducted to understand the anatomical causes for reduced hamstring muscle extensibility and its relation to both altered lumbopelvic movements and hamstring muscle injury. Muscle shortness refers to the length of the individual sarcomeres and their lengthening capacity. Muscle stiffness refers to the force required to effect the length of the connective tissue. These concepts focus directly on the structure of the muscle tissue and not on the neuro-mechano-sensitivity of the neural tissues for which muscles provide a dynamic container. (Kuilart, Woollam, Barling, & Lucas, 2005; Marshall, Cashman, & Cheema, 2011)
The anatomical causes for reduced hamstring muscle length and perceived tightness is the focus of this blog, with the aim to understand if altered neurodynamics or connective tissue extensibility is the cause of such tightness.
“Inability to extend the knee completely when the hip is flexed accompanied by discomfort or pain along the posterior thigh and/or knee is usually attributed to hamstring muscle tightness” (Mhatre, Singh, Tembhekar, & Mehta, 2013, p. 155). The hamstrings muscles are innervated by the sciatic nerve and also serve as a mechanical interface and container for the nerve. Therefore, both muscle tightness and altered neural tissue mobility can result in reduced knee extension range of movement and perceived muscle tightness.
“It is necessary to differentiate between various anatomical structures because the treatment of altered neural tissue mobility is conceptually different from that of reduced hamstrings extensibility”(Mhatre, et al., 2013, p. 154).
Kuilart, et al. (2005) found that 84% of patients with posterior thigh pain during a slump test experienced a reduction in symptoms with cervical extension. This evidence supports the hypothesis that subjects with perceived hamstring tightness were more likely to have neural mechanosensitivity than reduced hamstring length/extensibility (measured with the active knee extension test).
There is a growing body of evidence that indicates that hamstring flexibility is a reflection of neural tissue mechanosensitivity and that tests which allow structural differentiation are best suited to indicate the cause of reduced mobility and direct treatment towards neurodynamic techniques which focus on restoring optimal neurodynamics. (Butler, 2005; Lai, Shih, Lin, Chen, & Ma, 2012; Shacklock, 2005)
The first part of this blog outlines the physical examination and measurement of hamstring flexibility and neurodynamics of the sciatic nerve.
Measuring hamstring flexibility.
Almost all research articles use the Passive Straight Leg Raise Test (SLR) to measure hamstring flexibility. This test is describe in detail by Shacklock (2005), who states that >80 degrees hip flexion is a normal test outcome.
However, the SLR test does not measure hamstring muscle extensibility in isolation. It is a measure of muscle extensibility, neurodynamics and hip joint flexion range of movement.
The SLR test can be biased to differentiate more clearing between canal structures and peripheral nerves through structural bias, such as changing ankle dorsiflexion/plantarflexion, hip rotation/adduction/abduction, and cervical flexion. It is important to have a measure of the range of hip flexion at onset of symptoms, the location and description of the limiting factor and the effect that moving body parts distal/proximal to the hip has on the test outcome. From here it is easier to identify the role of neural mobility or muscle extensibility during the test.
Further examination may involve comparing the SLR test results to other tests such as the slump test and passive knee extension test (previously referred to as Lasegue test), and the active knee extension test.
Neurodynamic examination is designed to assess minor nerve disorders, which does not necessarily show conduction abnormalities but often accompany increased mechanosensitivity of the nerve. To gain information on whether neurodynamic responses participate in the mechanism of clinical symptoms, the structure differential manoeuvre could be added to glide the neural tissues and change the neural tension in question while minimising the movement of the musculoskeletal tissues in the target region. (Lai, et al., 2012).
Performing the tests...
Straight leg raise test
Maitland (2005) stresses the importance of consistency and reproducibility of the straight leg raise test and slump test. He describes a process of passive hip flexion, with full knee extension, slight hip adduction, no hip rotation and no pelvic lifting or rotation. Once the limit of range has been reached the dural structures can be placed under further stretch by adding ankle dorsiflexion and cervical flexion.
The order in which this test is performed can be varied to further bias structures and implicate or rule out the altered neurodynamics as a source of pain. For further description on structural differentiation and bias refer to Shacklock's text.
Slump Test
Use of the slump test is indicated for pain in any area of the body, but is most commonly used in the assessment of lower back pain. Maitland (2005) emphasises that the slump test is applicable to both lumbar and cervical spine disorders and should be included in the musculoskeletal assessment. Most importantly remember to ask for the pain response, pain location and relationship to the patient's problem. Then ensure to assess the change in pain response with release of cervical flexion.
"If forward flexion is restricted, it may be that the intervertebral joints are stiff or it may be that there is loss of movement of the structures in the canal or foramen. The tests that can be applied to move the structures in the vertebral canal without also moving the intervertebral joints are few in number" (Maitland, et al., 2005, p. 140).
Maitland (2005) & Shacklock (2005) instruct the process of a slump test as:
- Have the patient sit on the edge of the couch with the back of their knees touching the edge of the couch. Ask for resting pain/symptoms.
- Instruct the patient to slump through their upper and lower back (without flexing the cervical spine) and the therapist applies a gentle over-pressure (not to end of range). A good instruction is to ask the patient to slump their shoulders to hips and drop straight down. Assess for any change of symptoms.
- Instruct the patient to tuck their chin to chest as they look down and a firm overpressure is applied by the therapist to maintain cervical/thoracic/lumbar position. Assess for any change in symptoms.
- Instruct the patient to extend their knee as far as possible and note the range of symptoms or pain response. Ask "Is that your pain?".
- The end position is sustained while neck flexion is released and the change in pain response is noted. Also, if the patient is unable to achieve full knee extension, then once neck flexion is released, ask the patient to try extend their knee further.
- Ankle dorsiflexion can be added before or after knee extension to increase the stretch and assist with structural differentiation.
- If firmer over-pressure is required, repeat the test in long sitting.
- Therapists should also decide, based on the patient history, if over-pressure is appropriate at all. "The therapist must take into account specific information, such as irritability, sensitivity, latency and contraindications" (Shacklock, 2005, p. 143).
Positive response: Both the increased knee extension range and reduction in symptoms with release of cervical flexion would implicate dural pain-sensitised structures over hamstring muscle extensibility, as the limiting factor to knee extension range of movement.
Normal response (Maitland, 2005; Shacklock, 2005):
- Mid thoracic (T9/10) pain/discomfort during thoracic and lumbar flexion.
- A pain free lack of 30 degrees of knee extension can be normal.
- Stretching in the posterior thigh and knee, extending into the calf.
- Ankle dorsiflexion increases the posterior thigh/knee pain.
- Reduction of symptoms with release of cervical flexion.
A word of caution...
Maitland alerts therapists to the often-unpredictable response that patients with pain-sensitive canal structures and neural structures may have to the slump test or slump exercises. "Therefore, when the slump test is used as a technique, care must be taken on the first day and assessment over 24 hours is then necessary to determine whether the strength of the technique needs to be changed. If it is performed vigorously, an interval of 2-3 days should be left between treatments for soreness to settle so as to make accurate reassessment possible to determine how much has been gained" (2005, p. 149).
For variations in the slump test and passive straight leg raise test refer to Maitland's book Vertebral Manipulation, Shacklock's book Clinical Neurodynamics, and Butler’s book The Neurodynamic techniques (Butler, 2005; Hengeveld & Banks, 2005; Shacklock, 2005).
Passive knee extension test (Davis, Ashby, McCale, Mcquain, & Wine, 2005, p. 29).
Passive knee extension test
Subjects are positioned in supine and the hip is flexed to 90 degrees and stabilised. The therapist then passively extends the knee to the end of range, at which point, the knee flexion angle is measured. Their inter-rater reliability is reported to be 0.99 and some authors recommend the passive knee extensive test as the most reliable measure of hamstring length. (Davis, Quinn, Whiteman, Williams, & Young, 2008)
Normative data is limited but a rough guide for males is a knee flexion angle of 38 degrees and females 28 degrees across all ages (Kuilart, et al., 2005).
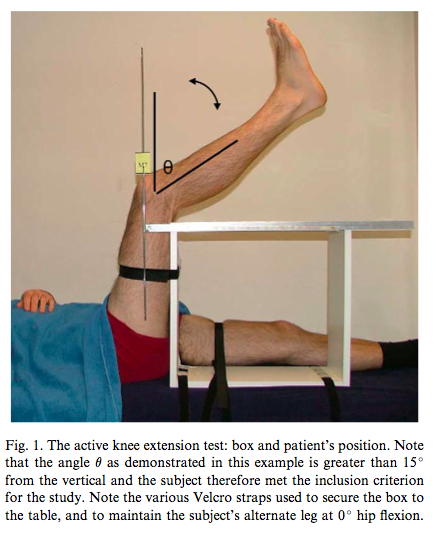
Active knee extension test (Kuilart, et al., 2005, p. 92).
Active knee extension test
“Subjects were positioned in supine without a pillow underneath the head. The participant’s left hip was flexed and stabilised to 90 degrees by an assistant. They were then asked to slowly extend their left knee until they felt the first stretch sensation. They maintained this position till the knee flexion angle was measured with the goniometer” (Mhatre, et al., 2013, p. 156).
Normative data suggests that a knee flexion angle of 40 degrees is the average range across ages and sexes (Kuilart, et al., 2005).
Are we measuring neurodynamics or muscle extensibility?
McHugh, Johnson, and Morrison (2012) established that when neural tension (thoracic and cervical flexion) is added to a hamstring stretch, the increased stretch sensation is not caused by contractile tissue response or increased EMG activity. The main changes in contractile response occur during the last 10 degrees of movement. Therefore neural tension is responsible for the increased stretch sensation during range. There results also demonstrated that when neural tension is increased during a hamstring stretch, there is likely to be a 9% decrease in range of movement in tolerable range with no difference in maximum stretch range.
These authors were the first to demonstrate in vivo that “in the absence of significant contractile activity, an increased resistance to hamstring stretch in the neural tension position can be attributed to tensile force in the neural structures” (McHugh, et al., 2012, p. 167).
What I learnt from this research is that:
- Many of the tests are not interchangable and a range of tests should be used to accurately measure range of movement and its limiting factor.
- Each test needs to be done in a reproducible manner.
- It is important to ask "Is that your pain?"
- Most of these tests allow for structural differentiation to explore neural tissue mobility and it's impact on the available range of movement.
- Assessment of causes of posterior thigh pain/tightness requires a neurodynamic examination.
The above tests have been well supported throughout the literature for their reliability and construct validity for the measurement of hamstring length and lower limb neurodynamics. Once the cause of reduced range and perceived tightness has been established, then treatment and exercises can be more specifically targeted to improve this deficit in range of movement.
The second part of this blog looks closer at the research comparing different treatments for improving ’perceived hamstring tightness’, the procedure for these techniques and their efficacy for improving hamstring flexibility and neurodynamics.
Sian
References
Butler, D. S. (2005). The neurodynamic techniques: a definitive guide from the Noigroup team: Noi Group.
Cleland, J. (2005). Orthopaedic clinical examination: an evidence-‐based approach for physical therapists: WB Saunders Co.
Davis, D. S., Ashby, P. E., McCale, K. L., Mcquain, J. A., & Wine, J. M. (2005). The Effectiveness of 3Stretching Techniques on Hamstring Flexibility Using Consistent Stretching Parameters. The Journal of Strength & Conditioning Research, 19(1), 27-32.
Davis, D. S., Quinn, R. O., Whiteman, C. T., Williams, J. D., & Young, C. R. (2008). Concurrent validity of four clinical tests used to measure hamstring flexibility. The Journal of Strength & Conditioning Research, 22(2), 583-588.
Hengeveld, E., & Banks, K. (2005). Maitland's peripheral manipulation: Elsevier/Butterworth Heinemann.
Kuilart, K. E., Woollam, M., Barling, E., & Lucas, N. (2005). The active knee extension test and slump test in subjects with perceived hamstring tightness. International Journal of Osteopathic Medicine, 8(3), 89-97.
Lai, W. H., Shih, Y. F., Lin, P. L., Chen, W. Y., & Ma, H. L. (2012). Normal neurodynamic responses of the femoral slump test. Manual therapy, 17(2), 126-132.
McHugh, M. P., Johnson, C. D., & Morrison, R. H. (2012). The role of neural tension in hamstring flexibility. Scandinavian journal of medicine & science in sports, 22(2), 164-169.
Shacklock, M. O. (2005). Clinical neurodynamics: a new system of musculoskeletal treatment: Elsevier Health Sciences.