The Pain Neuromatrix
"Anything that is detectable or accessible to the brain and relevant to the evaluation of danger to body tissue has the capacity to modulate pain. All contributing factors should be considered in all pain states". (Mr Alastair James Flett, APAM, FACP, 2014).
The most common complaint I assist people with is pain and I continually aim to expand my understanding on pain science in the hope of being able to better manage my patients and educate them about pain. The purpose of this blog is to highlight a few points I've read about the pain neuromatrix, which is only one piece of the puzzle when it comes to understanding the neuroanatomy and neurophysiology of pain.
Pain is defined by the IASP as "an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage" (International Association for the Study of Pain, 2014) .
What we've come to understand is that pain is not always a consequence to pathology/tissue damage and can occur in the absence of noxious stimulus (stimulus that is potentially threatening to normal body tissues) and nociception (the process of neural encoding of noxious stimuli) . Pain is an output from the brain which is multi-factorial and affected by multiple mechanisms.
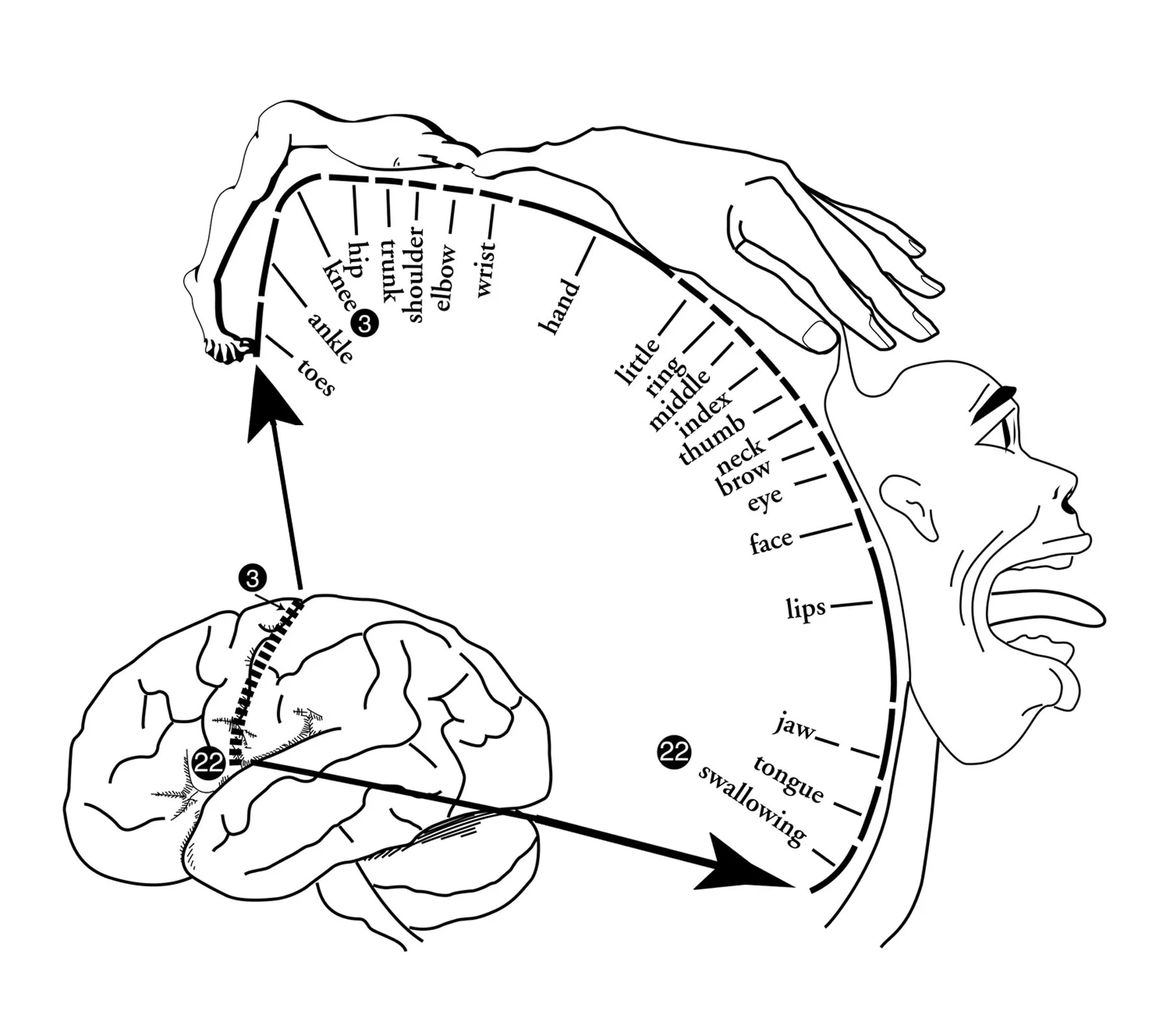
The image below demonstrates the pathway from nociception to pain and how the signal passes through the afferent nerves, to the dorsal root ganglion, then up the ascending pathways into multiple areas of the brain where it is processed and impacted on by the descending pathways to become the output of pain.
The mechanisms of pain (Courtesy of Medscape http://www.medscape.org/viewarticle/446350_3).
Neuromatrix
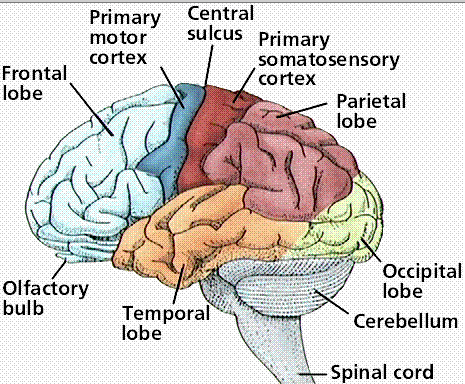
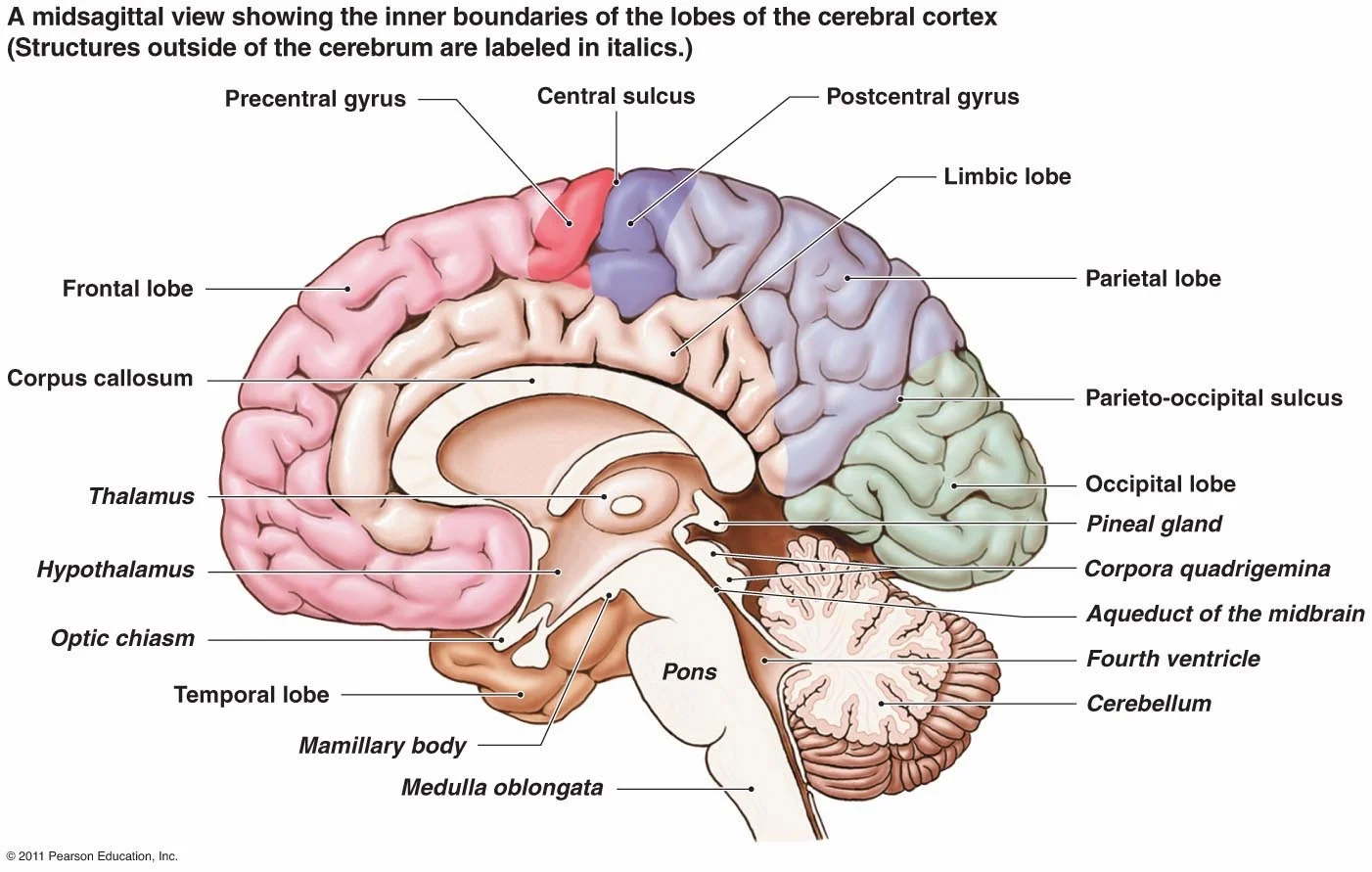
Pain is unpleasant and demands attention (Moseley, 2003). There is no single 'pain processing area of the brain', instead there is thought to be a series of neural connections known as the neuromatrix. The pain matrix is thought to consist of the dorsolateral prefrontal cortex, insula cortex, anterior cingulate cortex, primary and secondary sensory cortices, and the thalamus (Moseley, 2008). Every individual has a unique pain experience (an unique neuromatrix), but there are some areas of the brain (listed above) which are seen to be more frequently active on brain functional imaging.
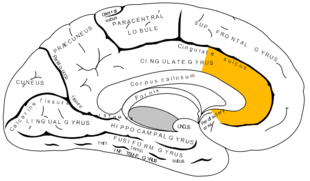
The anterior cingulate cortex is part of the cingulate gyrus and is thought to be responsible for autonomic functions (regulating heart rate and blood pressure) and cognitive functions (reward anticipation, decision making, empathy, impulse control and emotion). Moseley (2003) describes it as the action centre which causes humans to think "what should I do?" In relation to pain, the ACC is thought to provide an emotional description of pain and to coordinate an appropriate response.
The prefrontal cortex is part of the frontal lobe and involved in one's personality, specifically relating to planning complex cognitive behaviour, personality expression, decision making, and moderating social behaviour.
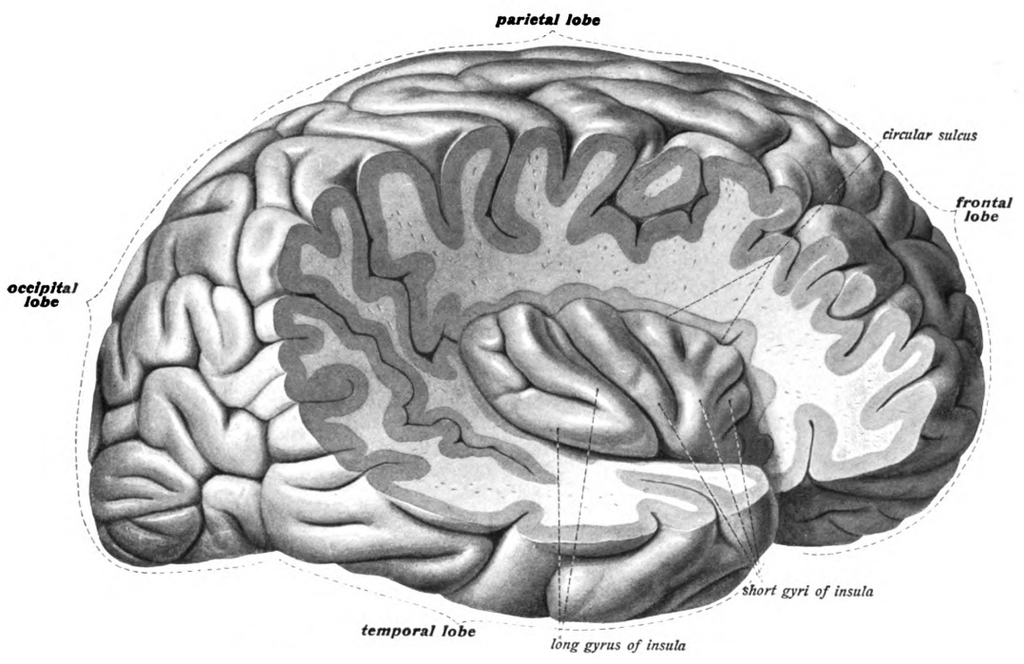
The insula cortex is found within the deep folds of the cerebral cortex and is involved in linking emotion to action. These functions may include perception, self-awareness, cognitive function, and motor control i.e it is involved in understanding the physiological functioning of the entire body.
The thalamus functions in relaying sensation, spatial sense and motor signals to the cerebral cortex, along with the regulation of consciousness, sleep and alertness.
The primary and secondary sensory cortices perceives and interprets sensations and touch. When being taught about the somatosensory cortex we learn about the homunculus (the mapping of regions on the body on the brain).
Although researchers are still exploring the neuroanatomy of pain, what I take away from this information is that many parts of the brain are involved in this 'neuromatrix'. This provides an explanation as to why everyone's pain experience is so individualised and also why chronic pain might lead to adverse effects on mood, cognitive function, sleep regulation, social interaction, self-esteem, and autonomic functions. Maybe that's why we are tackling pain with a 'bio-psycho-social approach'? If we address pain with only a patho-anatomical view point, we might miss the bigger picture....
Anterior cingulate cortex (ACC) courtesy of Google Images.
Insula
Primary and secondary somatosensory cortex
Homonculus
Thalamus
Prefrontal cortext (frontal lobe)
Two factors contribute to the chronicity of pain. Constant nocicpetion factors and constant non-nociception factors (cognitive-affective) which result in prolonged activate of the pain neuromatrix. "When pain persists, both the nociceptive system and the virtual body undergo profound changes, which increase sensitivity to noxious as well as non-noxious input and corrupt the integrity of motor output" (Moseley, 2003, p.132).
Prolonged activation of the neuromatrix leads to enhanced synaptic activity, enlarged receptor fields and reduced thresholds to previously non-noxious stimulus, up-regulation of signals by central mechanisms known as central sensitisation (IASP, 2014; Moseley, 2003). Physically patients begin to develop an unpredictable relationship between stimulus and pain output resulting in "difficult-to-predict flare-ups; poor tolerance of normal therapeutic approaches; problems with physical and functional upgrading; difficulty generalizing gains to other activities" (Moseley, 2003, p. 134).
How do we treat the neuromatrix in chronic pain?
Moseley proposed a desensitisation approach which aims to
- Reduce the threat of the input.
- Activate components of the neuromatrix without triggering the pain memory.
- Graded re-exposure to functional tasks.
1. Reduce the threat of the input.
Often we use manual therapy to reduce the noxious input contributing to the patient's pain problem. This approach is still suitable when combined with patient education regarding the purpose of the treatment. If they think they need treatment because "my tissues are still damaged" and the discomfort felt during such treatment is a cause of that damage, then this will not achieve the goal of reducing the threat of the input.
Education should focus on pain physiology. Anyone can learn about pain and understand the physiology, neuroanatomy and process of pain, and increasing people's understanding of pain is the first step to reducing the threat. Aim to educate your patients about the anatomy of pain, how chronic pain differs from acute pain, what the danger messages mean as this helps the patient to reconceptualise the meaning of pain.
You might be wondering how this is achievable when education can be time-consuming. Explain Pain is an excellent resource for patients and therapists and a great way to educate patients is to tailor this information to their particular story. For the sake of not getting bogged down on this topic lets move on and I hope to return to pain physiology in another blog.
2. Activating parts of the neuromatrix without triggering the pain memory.
It is important to gain an understanding of "previous tissue tolerance" and "current tissue tolerance" by asking the patient about their daily function, previous exercise, aggravating and easing factors etc. Determine how much input can be tolerated before the neuromatrix is activated (baseline).
Use the physical examination to observe the patient's current level of function and motor strategies to highlight any mal-adaptive movement/control strategies which might be contributing to their pain or preventing them from increasing their functional levels. A common example is over stabilisation of 'core' muscles with the belief that increased core strength results in reduced back pain.
If painful movements are identified then try to retrain these movements at a level which doesn't activate the neuromatrix. This might include:
- Breaking the task into smaller components, slower movements, less meaningful postures. We do this often when we break strength training up into isometric contractions, concentric and then eccentric exercises to retrain an impaired movement.
- Changing the context and environment the task is performed in to create a different neural-mapping for a similar movement e.g trunk flexion can be retrained by relaxing the body over a exercise ball.
- Change the posture of the task. We often do this with gait retraining and teaching people to control with pelvic tilt during phases of swing (hip extension/flexion during femur arcs in supine with control of pelvic tilt) and then reintegrating it back into walking.
- Imagine the movements being performed in a non-threatening context e.g turning the head into a cool breeze on a hot day rather than performing a head-check in heavy traffic. (Moseley, 2003). Another option is to use mirror therapy to use the non-affected side to visualise movement through the affected side.
3. Graded functional re-exposure.
Graded functional re-exposure to aggravating tasks is the final stage of neuromatrix-targeted-pain management (I made that word up). This part I think we are generally good at, taking a painful task and teaching the patient how to gradually build up a tolerance to that activity and promote good self-pacing techniques.
The article by Moseley (2003) goes into further depth on all these areas and even when I read it over and over again I learn something new. The main message I took away this time is that there are stages below our common assessment and rehabilitation techniques which can allow patients who suffer from chronic pain to improve their understanding of pain, to monitor their baseline and functional load, and to retrain painful movements. Sometimes we need to take another step back and break the task down into smaller components. It is also important to remember how complex the brain is and that everyone's is different and they neuromatrix provides an explanation on the individualisation of pain and why the bio-psycho-social approach to patient management is the current best way to practice physiotherapy in pain management.
Moseley (2003, p.130) expresses that "it is hoped that the astute reader will take from this work those aspects that can be integrated with their clinical experience and approach in order to promote better outcomes in a population for which success is elusive". I really like this statement as I feel it reflects the purpose of these ongoing blog posts and reflections.
Sian
References
Butler, D. S., & Moseley, G. L. (2013). Explain Pain:(Revised and Updated. Noigroup Publications.
Moseley, G. L. (2003). A pain neuromatrix approach to patients with chronic pain. Manual therapy, 8(3), 130-140.
Moseley, G. L. (2008). Pain, brain imaging and physiotherapy—Opportunity is knocking. Manual therapy, 13(6), 475-477.