Differential diagnosis of cervicogenic dizziness
Dizziness accounts for approximately 5% of presentations in primary care (Susanto, 2014). It has been reported to be present in up to 24% of patients with cervicogenic headache (Sjaastad & Bakketeig, 2008) and 75% in patients with chronic whiplash and associated disorders (WAD) (Treleaven et al., 2008). This blog post is the third part of a short series on dizziness. If you'd like to recap or read what was covered in previous blogs, go to cervicogenic dizziness and sensorimotor dysfunction and the distinguishing features of cervicogenic dizziness.
Dizziness can be categorised by the cause of dizziness: cardiac, psychological, medication induced, vestibular, metabolic, neurological, and cervicogenic. The purpose of this blog is to look at the conditions other than cervicogenic dizziness that cause either vertigo, pre-syncope, dysequilibrium and dizziness.
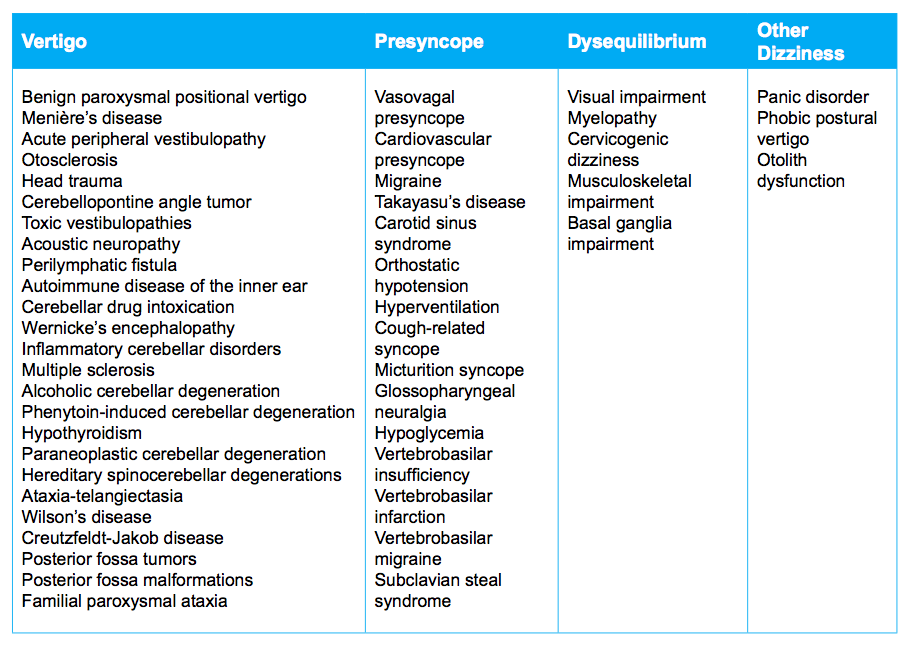
Conditions which cause vertigo, presyncope, and dysequilirbium (Schenk et al., 2006. p. E57).
The two most important conditions physiotherapists need to be able to recognise and be aware of are BPPV and VBI. The rest of the conditions discussed in this post are either more rare, less likely to present to physiotherapy as a primary case of dizziness, or just good to know about.
Benign paroxysmal positional vertigo (BPPV)
BPPV is the most common cause of peripheral vestibular dysfunction, with an incidence of 24% and most commonly seen between 50-70 years of age. BPPV can be insidious or traumatic in onset, and described as a feeling of vertigo, nausea, and vomiting elicited by head movements and changing position (particularly rolling over in bed).
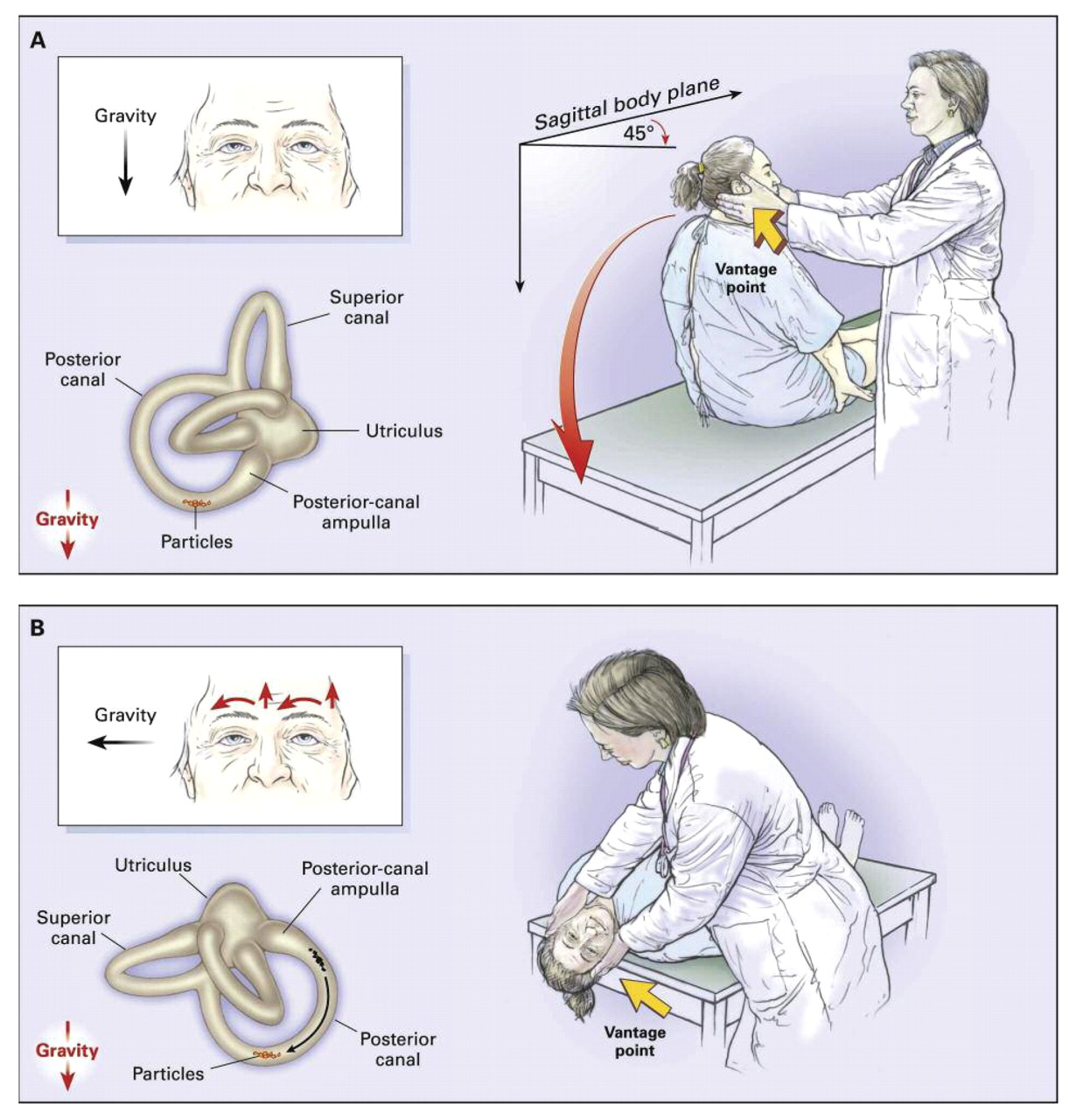
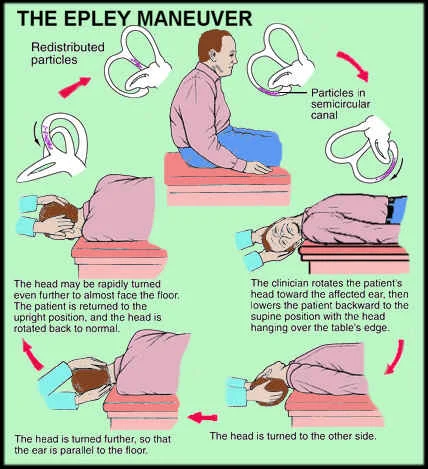
Nystagmus is another symptom which indicates a vestibular disorder. In BPPV nystagmus is generally latent and fatiguable. Central vestibular disorders have nystagmus too (which does not fatigue). In addition to reflex testing and assessment of the cervical spine, the Dix-Hallpike manoeuvre should be performed to assess the functioning of the semi-circular canals within the peripheral vestibular apparatus (Dispenza, et al., 2011). If you can’t reproduce the dizziness with physical examination or the Dix‐hallpike manoeuvre, then you can’t fix it using the Epley’s manoeuvre (Halmagyi & Halmagyi, 2000). More than often patients who suffer from BPPV will not demonstrate any other vestibular or auditory abnormality, which would be detected with inner ear pathology such as Meniere’s disease or Labarynthitis.
Dix-Hallpike manoeuvre (courtesy of Google images)
Images courtesy of Google images
Vertebral artery dissection
VBI is most commonly caused by vertebral artery stenosis (mainly atherosclerosis). The vertebral artery supplies the posterior circular of the brain, which supplies mainly the automatic parts of the brain such as the brain stem and cerebellum (Moubayed & Saliba, 2009). Vertebral artery insufficiency (VBI) is often accompanied by significant neurological deficits, with dizziness or vertigo often being the first noticeable symptom. If only one of the vertebral arteries is compromised and there is sufficient blood flow in the other, then the occlusion can be asymptomatic. If there is bilateral pathology however, then ischemia a rotational occlusion will occur if the neck is taken into rotation and extension.
All physiotherapists know about VBI because it is an part of the screening assessment performed prior to a progression of treatment to a grade 5 high velocity thrust technique for the cervical spine (i.e. risk assessment for cervical manips). There remains serious contention in the literature about the sensitivity, specificity and safely of performing the VBI clearing tests (this will most definitely be explored in a later blog). As far as clinical practice standards go, all Physios know that VBI screening exist, but not all Physios are comfortable performing the clearing tests due to the risks involved. But there many be other ways to assess the integrity of the vertebral arteries.
In the study by Moubayed & Saliba (2009) 49% of the participants that reported isolated dizziness or vertigo had hypoplastic or stenotic vertebral arteries on medical examination, which is a really high percentage of arterial disease. Most of these patients also had at least three stroke risk factors.
Thrombolic stroke risk factors include (Moubayed & Saliba, 2009, p. 2072):
- Age over 55
- Male sex
- Prior stroke or transient ischemic attack
- Ischemic heart disease
- Hypertension (treated or not)
- Diabetes (controlled or not)
- Lipid abnormalities (treated or not)
- Any cigarette smoking in past year
- Emotional stress
- Less than 4 hours of physical activity weekly
Neurological deficits and vestibular dysfunction were evaluated in this study (Moubayed & Saliba, 2009) with a variety of methods including a positional vertigo questionnaire, Dix-Hallpike test, Romberg test, electronystagmographic testing (ENG), and MRA imaging.
It was the first high quality trial to explore the pathology of VA and the correlation of dizziness/vertigo to VBI. Unfortunately the authors concluded that the sensitivity of examination is still too low (47%) (Moubayed & Saliba, 2009, p. 2075) . The consequences are VBI are too high to risk missing the opportunity for adequate medical treatment. The authors recommendation that imaging should be performed in all patients “suffering from isolated positional vertigo or dizziness of unexplained etiology and having at least three stroke risk factors" allowing for proper treatment to be initiated.
The aim of imaging is to examine the morphology of the vertebral arteries. The current gold standards for imaging include contrast-induced MRA and CTA. 'The sensitivity of MRA, CTA, and Doppler ultrasound is 93.9%, 100%, and 70.2%, respectively. The specificity for MRA, CTA, and Doppler ultrasound is 94.8%, 95.2%, and 97.7%, respectively' (Moubayed & Saliba, 2009, p. 2075).
Other conditions to consider
1. Pre-syncope is the sensation of fainting and can often be preceded by dizziness. It is caused by reduced cerebral perfusion, with cardiac disease being the common cause (Susanto, 2014). Patients with pre-syncope are more likely to report that their dizziness is not related to head movements or change in posture, because it is dependent on depletion of blood volume and can therefore occur at any time.
In the clinical setting, if you suspect that your patient is suffering not from dizziness related to vestibular or cervical origin, but cardiac, then taking a preliminary round of vital signs will help confirm your suspicions. These will include: blood pressure (in supine and standing), heart rate, respiratory rate, oxygen saturation, temperature and blood sugar levels. Referral to a GP or emergency room is the most common recommendation for this assessment.
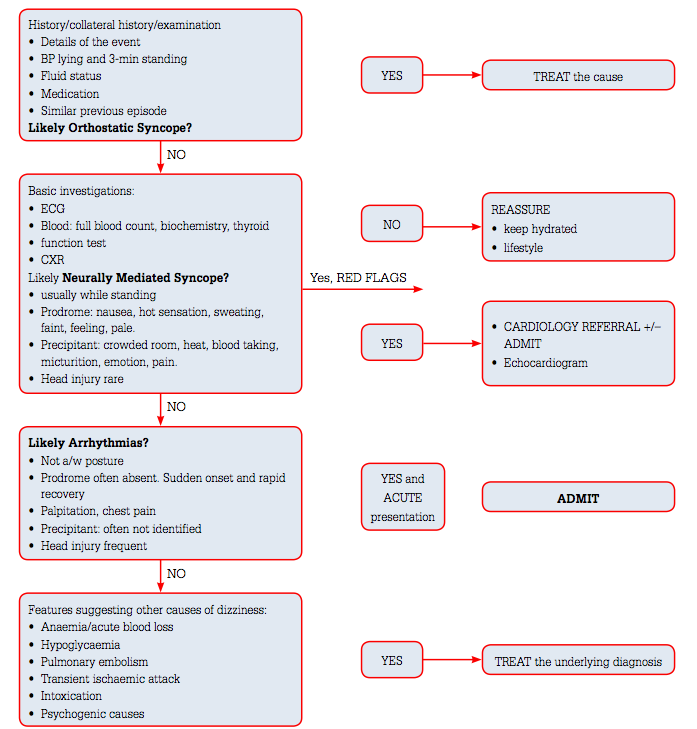
Symptoms associated with cardiac disease which patients may report to be present before, after or at the time of dizziness are chest pain, shortness of breath on exertion, and palpitation. They might have a part history of arrhythmias or cardiac disease. The episodes of syncope are short lasting and patients often make a full recovery following symptoms. Below is a flowchart of the decision making process in diagnosing pre-syncope.
Clinical decision making flowchart for pre-syncope (Susanto, 2014, p. 268).
2. Menier’s disease – “The presumed pathophysiological basis of Menière’s disease is episodic endolymphatic hypertension which produces devastating attacks of spontaneous vertigo with nausea and vomiting, together with a low frequency hearing loss, a low frequency tinnitus, and a sense of fullness or blockage in the affected ear” (Halmagyi & Halmagyi, 2000, p. 131).
3. Bilateral vestibular loss is a condition which is generally seen in the elderly patient and can be idiopathic in nature or caused by gentamicin oxotoxicity (medication toxicity). The main presenting symptoms are dizziness and a tendency for falls when vision is impaired. Aside from the medical evaluation, physiotherapy assessment will involve balance testing (with visual bias) and VOR reflex testing with head rotations. Treatment of bilateral vestibular loss is generally vestibular rehabilitation with a physiotherapist (Moubayed & Saliba, 2009).
4. Progressive supranuclear palsy (PSP) and other atypical parkinsonisms are another less frequent cause of disequilibrium. PSP often presents in the initial stages with dizziness and disequilibrium and is often misdiagnosed as Parkinson’s disease (PD). PSP is a neurodegenerative and progressive disease which results in progress loss of mobility and function. The physiological deterioration of this disease is similar to PD and the available treatment involved medication of idiopathic PD.
5. Mal de debarquement -aka disembarkment syndrome is the sensation of rocking, bobbing, swaying after being exposed to continuous movement eg. After flying or boat riding. I know what this symptom feels like because I experience it after getting off any boat or plane (and those playground roundabout things). There is no know cure and treatment often involves balance and vestibular retraining. So if you continue to feel symptoms of movement after disembarking from a plane, car, or boat, maybe you suffer from Mal de debarquement?
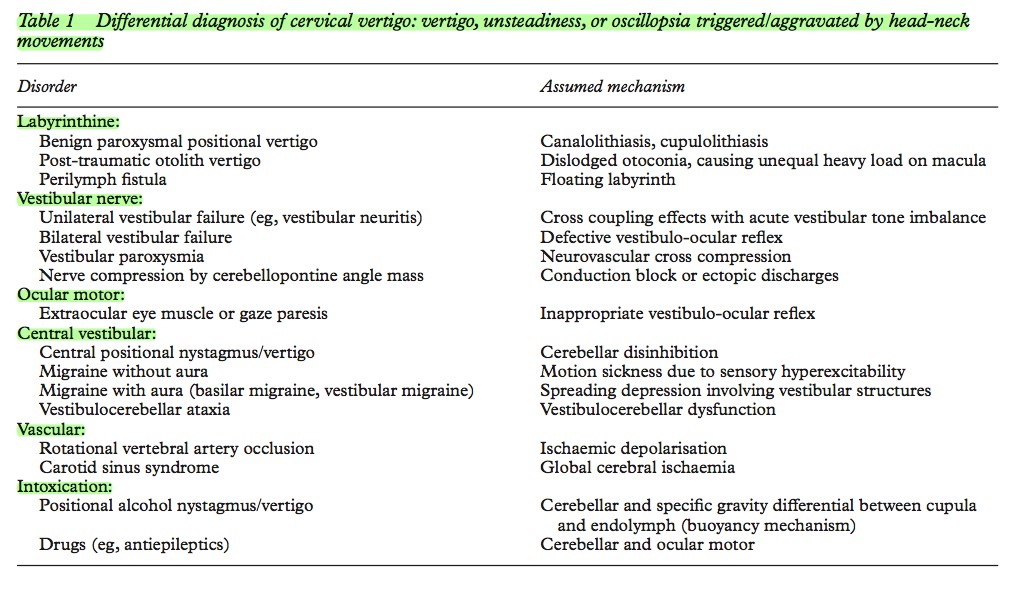
The table below outlines the differential diagnosis of cervical vertigo (know known as cervicogenic dizziness, vertigo, unsteadiness and oscillopsia). This article by Brant & Bronstein (2001) was an interesting read and great reference point.
(Brant & Bronstein, 2001, p. 8)
In summary, when you are questioning about general health, medical conditions, and red flags, it is helpful to keep some of these conditions in the back of your mind. It is not our role to be able to diagnose or differentiate between each one, but more to be confident in our clinical reasoning. Knowing what other medical professionals assess for can help with our communication of reasons for referral.
Now lets look at the physiotherapy intervention for cervicogenic dizziness & sensorimotor dysfunction. Following that I will conclude my blogs on this topic by exploring the specific research in the area of Whiplash Associated disorders.
Sian
REFERENCES:
Brandt, T., & Bronstein, A. M. (2001). NOSOLOGICAL ENTITIES?: Cervical vertigo. Journal of neurology, neurosurgery and psychiatry, 71(1), 8‐12.
Cherchi, M. (2011). Infrequent causes of disequilibrium in the adult. Otolaryngologic clinics of North America, 44(2), 405‐414, ix.
Dispenza, F., De Stefano, A., Mathur, N., Croce, A., & Gallina, S. (2011). Benign paroxysmal positional vertigo following whiplash injury: a myth or a reality? American journal of otolaryngology, 32(5), 376-380.
Halmagyi, G. M., & Halmagyi. (2000). Assessment and treatment of dizziness. Journal of neurology, neurosurgery and psychiatry, 68(2), 129‐134.
Moubayed, S. P., & Saliba, I. (2009). Vertebrobasilar insufficiency presenting as isolated positional vertigo or dizziness: A double‐blind retrospective cohort study. The Laryngoscope, 119(10), 2071-2076.
Schenk, R., Coons, L. B., Bennett, S. E., & Huijbregts, P. A. (2006). Cervicogenic dizziness: A case report illustrating orthopaedic manual and vestibular physical therapy comanagement. The Journal of manual & manipulative therapy, 14(3), E56‐E68.
Sjaastad, O., & Bakketeig, L. S. (2008). Prevalence of cervicogenic headache: Vaga study of headache epidemiology.Acta neurologica Scandinavica, 117(3), 173-180.
Sterling, M., Falla, D., Jull, G., Treleaven, J., & O'Leary, S. (2008). Whiplash, headache, and neck pain: research-based directions for physical therapies: Elsevier Health Sciences.
Susanto, M. (2014). Dizziness: if not vertigo could it be cardiac disease? Australian family physician, 43(5), 264.
Treleaven, J., Clamaron Cheers, C., & Jull, G. (2011). Does the region of pain influence the presence of sensorimotor disturbances in neck pain disorders? Manual therapy, 16(6), 636-640.
Treleaven, J., Jull, G., & Low Choy, N. (2004). Smooth pursuit neck torsion test in whiplash-‐associated disorders: relationship to self-‐reports of neck pain and disability, dizziness and anxiety. Journal of rehabilitation medicine, 37(4), 1‐1.
Treleaven, J., Jull, G., & Low Choy, N. (2005). Standing balance in persistent whiplash: a comparison between subjects with and without dizziness. Journal of rehabilitation medicine, 37(4), 224-229.
Treleaven, J., Jull, G., & Sterling, M. (2003). Dizziness and unsteadiness following whiplash injury: characteristic features and relationship with cervical joint position error. Journal of rehabilitation medicine, 35(1), 36‐43.
Treleaven, J., LowChoy, N., Darnell, R., Panizza, B., Brown-Rothwell, D., & Jull, G. (2008). Comparison of sensorimotor disturbance between subjects with persistent whiplash-associated disorder and subjects with vestibular pathology associated with acoustic neuroma. Archives of Physical Medicine and Rehabilitation, 89(3), 522-530.
Cervicogenic dizziness is often differentiated from vertigo and VBI, but there are many other conditions in which dizziness is a symptoms. Cherchi (2011) and Brandt and Bronstein (2001) provide a great outline for the less frequent causes of disequilibrium and the subtleties between each presentation. They are listed below with a few more common ones describes in further detail.