Does the audible pop matter? The neurophysiology of manipulation
Introduction
In the previous two blogs 'Chain reaction - the neurophysiological mechanism of manual therapy' and 'Neurophysiological mechanism of mobilisation' we discussed the current theoretical framework which explains what processes happen in the body when mechanical stimulation is applied to it. It is important to know the mechanisms of our effect with both mobilisation and manipulation, as it improves our understanding, acceptance, execution and teaching of these skills (Pickar., 2002).
"There are two ways of manipulating the conscious patient. The first, better thought of as mobilisation, is the gentler coaxing of a movement by passive rhythmical oscillations performed at the beginning, within or at the limit of range; the second is the forcing of a movement near that limit of range by a sudden thrust. The difference between these two techniques may seem negligible when comparing a strongly applied mobilisation with a gentle manipulative thrust, but there is an important difference: the patient can always resist the mobilisation if it should become too painful whereas the suddenness of the forceful manipulation prevents control by the patients”. (Maitland, 2005, p. 171)
This blog aims to review some of the literature surrounding spinal manipulation, as well as highlight the current barriers which have been identified for the low use of manipulation compared to other treatment options. As I read these articles I was surprised to find that my personal experience with learning and using 'manips' was a similar story to many other Physiotherapists.
Neurophysiology of manipulation
Pickar (2002) draws experimental data from many sources to explain the current hypotheses about mechanical and biomechanical effects of spinal manipulation. Within the mechanical model, it is speculated spinal manipulation can lead to ‘released meniscoids, releasing adhesions and reducing distortion of the annulus fibrosis’ (2002, p. 359). Further experimental support to justify this hypothesis.
“Whether spinal manipulation can alter neural function by mechanically changing compressional pressures or reducing the concentration of metabolites in the IVF is unknown” (Pickar., 2002, p. 362).
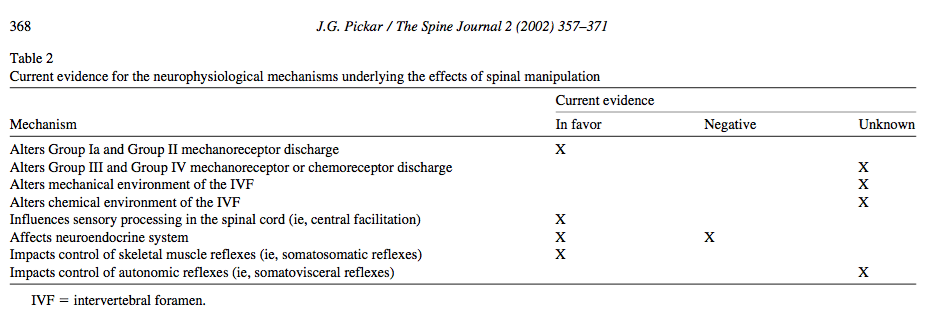
From a neurophysiological perspective, the previous blogs have highlighted the current ideas around the local, spinal and supraspinal effects of mechanical stimulation, which extend to both mobilization and manipulation. The table below, taken from Pickar (2002) indicates which hypotheses have supporting evidence. But what else do we know about the neurophysiological effects of a manip?
A summary of where the evidence lies regarding the neurophysiological mechanisms of spinal manipulation (Pickar, 2002, p. 368).
Hypoalgesia
Coronado et al (2012) conducted a systematic review to evaluate the hypoalgesic effects of spinal manipulation and the amount of reduction of pain intensity. From their systematic review they noted that many studies examining the hypoalgesic effects of spinal manipulative therapy (SMT) are on healthy participants.
The authors suggested that for our understanding of the effect of SMT on specific pain conditions to improve, we need to investigate SMT on clinical populations.
One interesting point from this systematic review is that reduced pain sensitivity is a widespread phenomenon, meaning that pain threshold is reduced throughout the body, not just at the anatomical site where the SMT was applied. A second point discussed in this review is that the hypoalgesic effect of SMT has only been shown to occur immediately after treatment and remains unclear the role SMT plays in long-term improvement. Finally, many of these studies do not provide a link between changes in pain sensitivity and changes in clinically relevant outcome measures. When referring to pain sensitivity, the only consistent measure used between studies is pain pressure threshold and it is still uncertain if there is the same impact on temperature and chemical pain thresholds. Many studies also fail to discuss dosage of SMT, which remains a relatively undefined aspect of manual therapy. So we know that manipulation has a local and widespread ability to improve pain pressure threshold and provides an immediate reduction in pain sensitivity.
Audible Pop (AP)
One of the defining characteristics of a high-velocity, low-amplitude (HVLA) thrust technique is the presence of an audible pop (AP). Although the noise can be very satisfying to both the clinician and the patient, there is evidence which currently questions it’s clinical significance.
“HVLA manipulation is associated with hypoalgesia to Aδ fiber-mediated pain and temporal summation regardless of whether an AP is perceived” (Bialosky, Bishop, Robinson, & George., 2010, p. 121).
In both the lumbar and thoracic spine, studies have shown that there is no improved effect of a manipulation on pain and range of movement if there is a audible pop (Bialosky, et al., 2010; Sillevis & Cleland., 2011). That means that performing the technique still counts whether you ‘crack it’ or not.
“Cavitation is the formation or release of gas from the synovial fluid within the joint caused by separation of joint surfaces resulting in an intracapsular reduction in pressure” (Sillevis & Cleland., 2011, p. 37). It is speculated that the gas within the synovial joint causes an elongation of mechanoreceptors during the technique which causes a depolarization of mechanoreceptors. This depolarization can result in muscle relaxation and improved range of movement, as well as activation of the dorsal horn in the spinal cord, thought now to contribute to descending spinal pain inhibition. There is also going to be an immediate effect on the autonomic nervous system (Pickar., 2002; Sillevis & Cleland., 2011).
Something new that I learnt while reading these articles is that the pupil receives both sympathetic and parasympathetic innervation. Therefore the change in pupil diameter following manipulation is a direct reflection of the sympatho-excitatory effect of the technique. Hypothetically, you would observe pupil dilation if the sympathetic nervous system was stimulated following the manipulation.
Sillevis & Cleland (2011) also conducted a study to explore if the audible pop has an impact on pain reduction but also looked at the effect on the autonomic nervous system. They used a T3-4 thoracic AP thrust on a population of chronic neck pain people.
After applying a thoracic AP thrust technique, the presence of a pop has no direct impact on sympathetic nervous system excitation and it is speculated that the increased perceived benefits are more likely a placebo effect based on the patient's expectations from the manipulation.
It is therefore important to educate to your patients that the presence of a pop doesn’t make the treatment more or less effective and that performing the manipulation is what gives the pain-relieving effect. This certainly is a tough belief to challenge but worthwhile topic to approach with your clients. Furthermore, Sillevis & Cleland emphasised that clinicians “should not use the presence of an audible pop as an indication that the manipulation technique was successful” (2011, p. 47).
“Manipulation is characterised as a high velocity and low amplitude movement”, not by the presence of an audible pop (Bishop, Beneciuk, & George., 2011, p. 440).
Temporal sensory summation (TSS)
Bishop, Beneciuk & George (2011) investigated the effect of spinal manipulation on temporal sensory summation (TSS), a component of central sensitisation that occurs when rapid repeated stimulation is applied, with reported pain levels increasing. Temporal sensory summation is thought to occur at the level of the dorsal horn and cerebral cortex in areas involved in pain processing. It is a behavioural measure of ‘wind up’ in the central nervous system, commonly displayed by patients suffering from chronic pain conditions (Bishop, Beneciuk & George, 2011, p. 444). Wind up is a temporary adaptation in the central nervous system in response to repeated stimulation, however synaptic changes occur in chronic pain conditions that lead to sustained TSS. In this particular study, they investigate the effect of a thoracic manipulation on upper extremity and lower extremity pain pressure threshold, and measure TSS through the application of 10 hot heat packs. What they noticed is that following thoracic manipulation there is an immediate reduction in TSS in healthy subjects. Further research is still required to investigate the effect of manipulation on TSS in clinical populations.
So we are starting to build this picture that spinal manipulation has a local and widespread hypoalgesic effect, regardless of an audible pop. That pop however, might increase the placebo effect but it doesn't determine if a treatment was successful or not. The success of a manipulation comes down to handling and execution.
From previous blogs, we know mechanical stimulation has an effect on the dorsal root ganglion and periaquaductal grey (along with other areas) causing a descending inhibitory effect on pain. Manipulation can also have an effect on temporal sensory summation a.k.a windup but needs to be investigated in clinical populations with chronic pain conditions. As the research evolves, we hope to improve our understanding of how manipulation (manips) works with the hope of explaining the treatment effect better to our clients, understanding how they work, and improving our acceptance and use of these techniques. As Flynn, Wainner & Fritz explain “despite evidence that suggests manipulation is an effective and potentially cost-saving intervention for patients with LBP, it seems to be under-utilised by physical therapists, when compared to utilisation rates of other interventions that have little to no evidence to support their use” (2006, p. 578).
In fact, some studies have shown that 30% of Physiotherapist's believed spinal manipulation to be an effective treatment, yet, when compared to other treatment modalities, spinal manipulation is used in only 3-4% of cases (Li & Bombardier, 2001).
BARRIERS TO USING MANIPULATION
What is causing this dramatic drop and utilisation of this technique? Is it confidence, technique, clinical outcomes? A suspected reason for the low use of manips is there is a lack of understanding about how it works, a lack of confidence in performing the technique, and the controversy around gaining Informed Consent (which I hope to cover in a separate blog).
Flynn, Wainner & Fritz (2006) present a curriculum model for teaching spinal manipulations which involves the following steps. I'm going to expand on the first two.
- Clinical reasoning
- Skill acquisition
- Determination of outcomes
Skill assessment and practical examination
1. Clinical reasoning
Based on what the last two blogs have covered about the mechanical and neurophysiological effects of spinal manipulative therapy, we can start to realise that the clinical reasoning process of manual therapy is fairly in-depth. The first step in teaching manipulation is to teach Physiotherapists how to pick a patient is likely to have a favourable response to this treatment modality.
There are are times when techniques fail to help a patient. Either the technique was not executed appropriately, the patient was inappropriately selected for the treatment, or the condition was non responsive to treatment (Bialosky et al, 2009; Maitland, 2005).
“It is important that, with every technique, the manipulative physiotherapist must be fully aware, at all times of the effects the technique is having not the patient’s symptoms while the technique is being performed” (Maitland, 2005, p. 180) Within this clinical reasoning process it is important to think about the following aspects of selecting a technique:
- Mobilize or Manipulate?
- Direction of movement
- Position in which the direct movement would be performed
- The manner of the treatment
- The duration of the treatment
Other aspects of clinical reasoning not related to selection of technique revolve around our understanding of the problem and the technique. We need to know what the treatment is trying to achieve and the mechanisms behind the response involved. Once we know this, we can decide if the patient and the treatment are a compatible combination. We are constantly brought back to the indications and contraindications for treatment.
What are the contraindications to manipulation?
- Presence of signs/symptoms that indicate serious pathology which includes
- Malignancy - primary or secondary
- Inflammatory conditions, eg osteomyelitis, tuberculosis
- Spinal cord compression
- Cauda equina compression
- Recent fractures
- Osteoporosis
- Vertebral artery insufficiency
- Ankylosing Spondylitis - in active stage
- Rheumatoid arthritis - never manipulate upper cervical spine
- Spondylolisthesis - if symptoms are arising slip
- Gross foraminal encroachment
- Acute nerve root compression or irritation
- Teenagers and children
- Spasm
- Instability
- Psychological pain
- Undiagnosed pain
- Last trimester of pregnancy
- Recent whiplashes
- Haemophilia or patients on anti-coagulants
- Take special care with
- Severe pain
- unstable conditions
- Acute nerve root pain
- Irritable conditions
- Signs suggest worsening nerve root compression
- If mobilisation reproduces distal symptoms
- Worsening conditions
Another aspect in the clinical reasoning process which should never be overlooked or underweighted is the experience of the patient. Ask your patient…. What has worked in the past? How have you responded to spinal manipulation previously? Do you normally crack your neck and back by yourself? Have you had any poor experiences. Asking the patient is one of the quickest ways to direct your clinical reasoning.
For example: if they have had acute back pain in the past and responded well to a manip, they might be expecting this form of treatment again. But, what if you decide it’s contraindicated this time round because now they have pain radiating down they posterior leg. You need to explain yourself and why you feel it is unsafe and also educate the patient so they don’t just go off to the next person seeking an adjustment.
Another example could be if a patient comes in with headaches and complains of a stiff neck. You ask what treatment has worked in the past and they reply neck massage and cracking my back between my shoulder blades. Perhaps if this was a day 1 assessment, you might err on the side of caution with performing multiple treatments and a manip on the first day? But after treating their neck the results just aren’t as good as you hopped. Based on your assessment and their past history, you perform a T3/4 AP HVT and suddenly their neck rotation is significantly better. But all the while, you had a reasoning process to help you decide if this was the right path to take or not.
Without a clinical reasoning process, the skill is dangerous. It can’t be used on everyone.
2. Skill acquisition
We began learning manipulation techniques during our undergraduate degree. Interestingly, as confident as you become practicing on your peers, it is a totally different situation when you perform them on a ‘live patient’. Reflecting on this now, I did not perform a single manip during my undergraduate and post graduate clinical placements. Really? 4 years of clinical placements in hospitals and not one of them were suitable for a manipulation? What does this say?
For me, I got my practice through my work. First on my colleagues and then I incorporated it more and more into clinical practice. Now the idea of manips doesn’t scare me like it used to. But if others followed a similar path and never worked in a clinic where mentors were such proficient manipulators and great teachers, maybe they would never practice it again? The concept I needed to master first was my understanding of movement diagrams, followed by practicing my handling skills.
Interestingly, my experience is not uncommon. Struessel et al (2012) conducted an American study which found that the biggest barrier to using manipulation was based on their experience with clinical placement. If students didn’t practice during clinical placements, either because their clinical instructor wasn’t confident, or the patient’s weren’t suitable, then they were much less likely to perform these techniques once graduated.
When I was going through my Master’s degree, I knew that learning to be an experienced and skilful manipulative therapist was one of the primary goals and expectations. I practiced under supervision twice a week for the entire second year, as well as multiple times a week independently with other students and my colleagues. Within the final year of my masters I went from someone who rarely manipulated much more than the occasional thoracic spine to implementing it on most days. I also got involved teaching on the Spinal level 1 & 2 courses, passing my knowledge and experience onto other Physiotherapists.
Interestingly, learning how to perform manipulations also taught me to use PPIVMS more frequently in my treatment. I think the repetitive practice of handing with a cradle hold and chin hold allowed both my mobilisations and manipulations to become more accurate. There was a spill-over effect in technique improvement.
I enjoyed learning about the contraindications and indications as well as the step-by-step procedure for each technique, as with an increased understanding, my execution and clinical reasoning improved. I’ve been able to pick more accurately which patients will benefit from a manip and which ones won’t. Overall this makes my clinical outcome better and because I get better results, my confidence improves. I’ve changed my understanding of manips and no longer view it as a forceful and dangerous technique. It is more about set up, a quick thrust and picking the right person. I’ve also changed the language I use to describe manips – which probably enhances the placebo effect or at least reduces the nocebo effect I have on patients.
You need to practice independently so much more that what the educational courses allow. For me personally, I tried to practice most days, although that was hard. The manips I focused on were the lumbar rotation manip, Thoracic (both AP and screw), cervical C23 rotation manip, and cervicothroacic junction. Although we were taught up slopes, down slopes, upper cervical manips and more, I always found that when I was treating patients in these regions, if I combined physiological movements during mobilisation that I could clear the movement before a manip was required. But without the combined movements, I wouldn’t have know how to keep hunting.
Conclusion
Spinal manipulative therapy has the ability to reduce pain both locally where it is applied and widespread. It has a mechanical effect locally on the tissues as well as an effect on spinal and supraspinal mechanisms. Interestingly, the audible pop doesn't seem to matter as much and it's effect is still largely unclear. If you don't hear a pop it certainly doesn't mean the treatment failed. Many Physiotherapist's struggle with manips or avoid them all together. Perhaps this reflects how they are being taught in undergraduate institutions? If we don't understand something, we are less likely to use it. And as the old saying goes, if you don't use it you lose it. My attitude towards manips has changed dramatically since completing my Masters in Musculoskeletal Physiotherapy. I now feel more knowledgable and confident with my handling and clinical reasoning. But not without significant amounts of practice. My advice, talk to your mentor about building in regular practice into your week, take post-graduate courses that help correct and refine your technique, and don't forget how much you'll learn just from practicing the handling and movement of PPIVMS. Anecdotally, I've seen the dramatic effect manips can have on treatment outcomes and I urge you to explore these benefits further yourself.
Sian
References:
Bialosky, J. E., Bishop, M. D., Robinson, M. E., & George, S. Z. (2010). The relationship of the audible pop to hypoalgesia associated with high-velocity, low-amplitude thrust manipulation: a secondary analysis of an experimental study in pain-free participants. Journal of manipulative and physiological therapeutics, 33(2), 117-124.
Bishop, M. D., Beneciuk, J. M., & George, S. Z. (2011). Immediate reduction in temporal sensory summation after thoracic spinal manipulation. The Spine Journal, 11(5), 440-446.
Boissonnault, W., & Bryan, J. M. (2005). Thrust joint manipulation clinical education opportunities for professional degree physical therapy students.Journal of Orthopaedic & Sports Physical Therapy, 35(7), 416-423.
Coronado, R. A., Gay, C. W., Bialosky, J. E., Carnaby, G. D., Bishop, M. D., & George, S. Z. (2012). Changes in pain sensitivity following spinal manipulation: a systematic review and meta-analysis. Journal of Electromyography and Kinesiology, 22(5), 752-767.
Flynn, T. W., Wainner, R. S., & Fritz, J. M. (2006). Spinal manipulation in physical therapist professional degree education: A model for teaching and integration into clinical practice. Journal of Orthopaedic & Sports Physical Therapy, 36(8), 577-587.
Maitland, G. D. (2005). Maitland's vertebral manipulation (Vol. 1). E. Hengeveld, K. Banks, & K. English (Eds.). Butterworth-Heinemann.
Pickar, J. G. (2002). Neurophysiological effects of spinal manipulation. The Spine Journal, 2(5), 357-371.
Sillevis, R., & Cleland, J. (2011). Immediate effects of the audible pop from a thoracic spine thrust manipulation on the autonomic nervous system and pain: a secondary analysis of a randomized clinical trial. Journal of manipulative and physiological therapeutics, 34(1), 37-45.
Struessel, T. S., Carpenter, K. J., May, J. R., Elizabeth Sampey PT, D. P. T., & Mintken, P. E. (2012). Student perception of applying joint manipulation skills during physical therapist clinical education: Identification of barriers. Journal of Physical Therapy Education, 26(2), 19.
Snodgrass, S. J., Rivett, D. A., Robertson, V. J., & Stojanovski, E. (2010). Cervical spine mobilisation forces applied by physiotherapy students.Physiotherapy, 96(2), 120-129.