Risk Factors and assessment of hamstring muscle strain injury
Prevalence, incidence and etiology
Hamstring muscle strain injuries (HMSI) are common in sports that involve sprinting (Orchard et al., 1997), acceleration, deceleration, rapid change in direction and jumping (Devlin, 2000; Drezner, 2003). For this blog, Grant Freckelton discusses the prevalence, etiology, and identification of risk factors for such injuries based on a research paper he was involved in in 2013.
These injuries can result in substantial time lost from sport and commonly recur (Orchard & Seward, 2008; Upton et al., 1996). In the Australian Football League (AFL) hamstring injuries are the most prevalent injury with a 21 years of age, with a mean of 6 new injuries per club per season causing 20.4 missed matches per club per season. There is also a high average recurrence rate of 26% (Orchard et al., 2013).
Hamstring injuries during sprinting are proposed to occur during the terminal swing phase of running as a consequence of an eccentric contraction (Schache et al., 2009; Heiderscheit et al., 2005). Askling, et al., (2006) has proposed two distinct mechanisms of hamstring injuries.
- Type 1 involve high intensity runningwith injury occurring during late swing phase involving the proximal musculotendinous junction of the long head of biceps femoris.
- Type 2 is described as a stretching of the hamstring complex due to extreme joint positions involving mostly semimembranosus and the proximal tendon (Yu et al, 2008; Askling et al, 2006).
The majority of hamstring injuries occur at the biceps femoris (BF) long head (Koulouris & Connell, 2005; De Smet & Best, 2000; Croisier, et al., 2004). During the 2011 AFL season 84% of all hamstring injuries occurred at biceps femoris, 10% at semimembranosus and 4.3% at semitendinosus (Pizzari et al. 2012). Of these 27.3% of all hamstring strains occurred at the distal musculotendinous junction (MTJ) of BF, 19.7% at proximal MTJ of BF and 18.2% in the belly of BF (Pizzari et al. 2012).
Risk factors
Many papers have examined potential risk factors for HMSI, with age and previous hamstring strain being accepted as risk factors, and many others inconsistently identified as contributing to the injury. A systematic review and meta-analysis into risk factors for hamstring injury identified older age, increased quadriceps peak torque and past history of hamstring injury were associated with increased risk of hamstring muscle strain injuries. Other strength measures such as hamstring:quadriceps ratio, commonly perceived to be predictive of injury, were not associated with hamstring injury (Freckleton & Pizzari, 2013).
(Cleland, 2005, p.249)
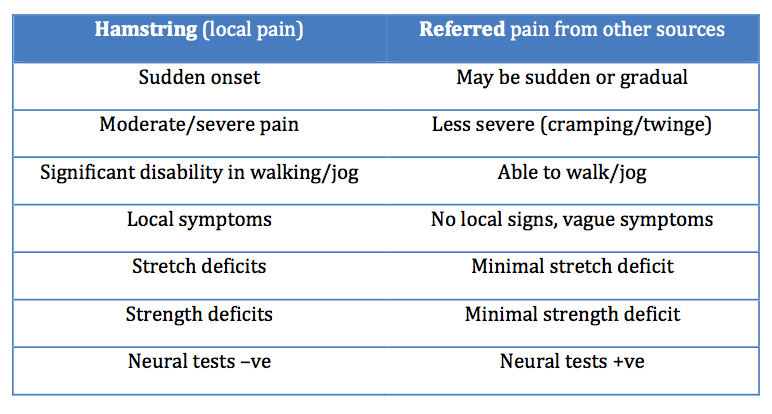
Clinical assessment and Differential diagnosis
Due to multiple possible causes of posterior thigh pain, accurate assessment and diagnosis is critical for appropriate treatment to be implemented. Possible sources of posterior thigh pain not limited to, but include lumbar spine (disc/ facet joint), hip, SIJ, gluteal/piriformis/gemelli trigger points, tendonopathy, avulsion injuries, vascular claudication and compartment syndrome (Brukner & Khan, 2006).
The subjective assessment is key to correctly diagnose an injury. Players with a hamstring injury will report sudden onset of pain localised to the hamstring region with a clear mechanism or incident. There is significant disability at time of injury (Pizzari, et al., 2010). Previous injury history, particularly previous hamstring injury is also important, as this is one of the major risk factors for future hamstring injuries (Freckleton, et al., 2012).
Clinical examination for determining hamstring injury is considered to be reliable and accurate (Schneider-Kolsky, et al., 2006). A hamstring injury can be defined as having positive clinical signs and symptoms including (Bennell, et al., 1999):
- Immediate onset of posterior thigh pain,
- Tenderness on palpation,
- Reproduction of pain on stretch of hamstring,
- Reduced straight leg raise ROM,
- Reproduction of pain and reduced strength on resisted active contraction of hamstrings, and
- Unable to continue playing or training and miss at least one game due to the hamstring injury.
The physical examination should include lumbar spine AROM, Slump, SLR, active knee extension test (AKE), passive hamstring muscle stretch and palpation of pelvic musculature for trigger points and reproduction of posterior thigh pain. Resisted contraction of the hamstrings should be tested in multiple positions of knee flexion (Brukner & Khan, 2006). Palpation is the most important aspect of the physical examination to help identify location and severity of the injury (Pizzari, et al., 2010).
(Brukner & Khan, 2006)
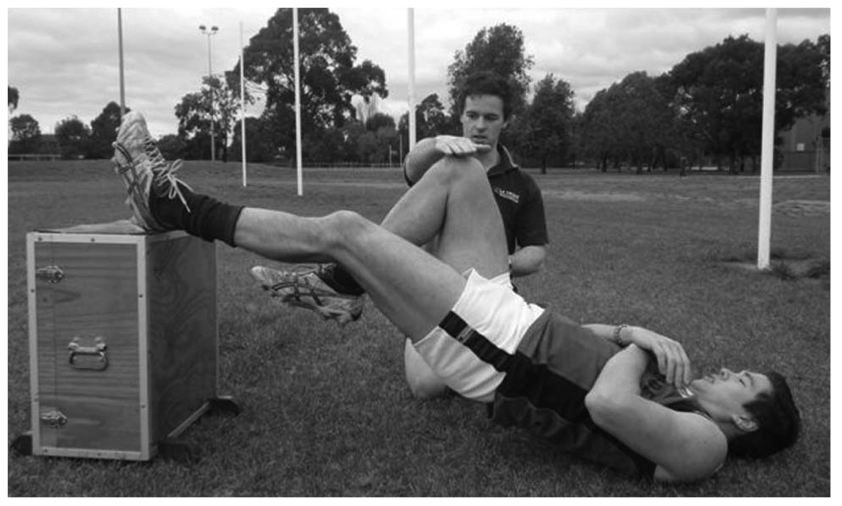
A recent study investigated the use of the single leg hamstring bridge (SLHB) as a clinical test in predicting hamstring injuries in football players. The single leg hamstring bridge tests the hamstring muscles in a functional position similar to terminal swing and assesses endurance parameters rather than peak torque. This study demonstrated a significant deficit in preseason SLHB scores on the right leg of players that subsequently sustained a right-sided hamstring injury.
Age, previous knee injury and a history of hamstring injury were other risk factors supported in the study, which also had a negative impact on SLHB scores. Due to the confounding variables and low injury rate in this study, further research is required (Freckleton, et al., 2013). The SLHB test could be used to screen and identify athletes who are potentially at risk of sustaining a hamstring injury. It may also be used to evaluate the readiness of an athlete to return to sport.
Grant Freckleton assessing hamstring muscle strength using the single leg hamstring bridge.
Grant Freckleton (author)
References
Askling, C., Saartok, T., & Thorstensson, A. (2006). Type of acute hamstring strain affects flexibility, strength, and time to return to pre-injury level. British Journal of Sports Medicine, 40(1), 40-44.
Bennell K, Tully E, Harvey N. Does the toe-touch test predict hamstring injury in Australian Rules footballers? Aust J Physiother 1999;45:103–9.
Brukner, P., & Khan, K. (2006). Clinical sports medicine. McGraw Hill.
Croisier, J. L. (2004). Factors associated with recurrent hamstring injuries. Sports Medicine, 34(10), 681-695.
De Smet, A. A., & Best, T. M. (2000). MR imaging of the distribution and location of acute hamstring injuries in athletes. American Journal of Roentgenology, 174(2), 393-399.
Devlin L. Recurrent posterior thigh symptoms detrimental to performance in rugby union: predisposing factors. Sports Med 2000;29:273–87.
Drezner JA. Practical management: hamstring muscle injuries. Clin J Sport Med 2003;13:48–52.
Freckleton G, Pizzari T. Risk factors for hamstring muscle strain injury in sport: a systematic review and meta-analysis. Br J Sports Med 2013;47:351–8.
Freckleton, G., Cook, J., & Pizzari, T. (2013). The predictive validity of a single leg bridge test for hamstring injuries in Australian Rules Football Players. British journal of sports medicine.
Heiderscheit BC, Hoerth DM, Chumanov ES, et al. Identifying the time of occurrence of a hamstring strain injury during treadmill running: a case study. Clin Biomech 2005;20:1072–8.
Koulouris, G., & Connell, D. (2005). Hamstring Muscle Complex: An Imaging Review1. Radiographics, 25(3), 571-586.
Orchard J, Marsden J, Lord S, et al. Preseason hamstring muscle weakness associated with hamstring muscle injury in Australian footballers. Am J Sports Med 1997;25:81–5.
Orchard J, Seward H. The AFL Injury Report 2008. Australian Football League 2008.
Orchard J, Seward H. Orchard MJ. The AFL Injury Report 2012. Australian Football League 2013.
Pizzari, T., Wilde, V., & Coburn, P. (2010). Management of hamstring muscle strain injuries in the Australian Football League (AFL): A survey of current practice. Journal of Science and Medicine in Sport, 13, e76.
Pizzari, T., Taylor, R., & Coburn, P. (2012). The who, where and how.. Understanding hamstring injuries in the AFL. <em>Journal of Science and Medicine in Sport, S143.
Schache AG, Wrigley TV, Baker R, et al. Biomechanical response to hamstring muscle strain injury. Gait Posture 2009;29:332–8.12
Schneider-Kolsky M, Hoving J, Warren P, et al. A comparison between clinical assessment and magnetic resonance imaging of acute hamstring injuries. Am J Sports Med 2006;34:1008–15.
Upton PA, Noakes TD, Juritz JM. Thermal pants may reduce the risk of recurrent hamstring injuries in rugby players. Br J Sports Med 1996;30:57–60.
Yu, B., Queen, R. M., Abbey, A. N., Liu, Y., Moorman, C. T., & Garrett, W. E. (2008). Hamstring muscle kinematics and activation during overground sprinting. Journal of biomechanics, 41(15), 3121-3126.