The continuum from preventative to rehabilitative care
Reflecting on a weekend of teaching I noticed a common theme as I transitioned from participating at the UCSF sports medicine conference to teaching an advanced track seminar at the NATA annual conference. This theme is something I've been brought back to over and over again, the continuum and transition between preventative and rehabilitative care.
What I loved about the UCSF conference was the interconnection between surgeons and doctors, and their audience of athletic trainers and physical therapists. This interdisciplinary education is a unique trait to the continuing education I've encountered in the USA. The presenters continued to emphasize that our role with patients is to allow for healing of damaged tissues, provide educations, confidence and encouragement, and to ensure that a safe and graded process of return to sport does occur. Too many people are being rehabilitated to the recovery of pain and strength and the functional demands of returning to sport are overlooked.
These presenters reinforced that we continue to struggle with injury prevention that results from poor knowledge of training loads and neuromuscular development across age groups. One of our biggest challenges is sharing enough knowledge through all levels from parenting, coaching and rehabilitation to ensure athletes are safe and well managed. There was a large focus also on keeping a clear perspective on the psychological and biological factors which impair healing and recovery, especially sleep. Who owns the sleep domain remains unclear, but as our understanding of sleep and the impact of sleep deprivation has on the body, mind and physical performance increases, the demand and responsibility might land with our profession. And we need to be ready and prepared to question about sleep quality, evaluate its importance and provide sleep strategies or provide quality referrals to assist our patients in optimizing their recovery path.
Again that word recovery rears it's head. Would it not be easier to prevent such issues such as sleep deprivation from occurring if we could just educate the direct customer? This is where another great challenge lies. The sharing and distribution of important knowledge about health and fitness, while ensuring that our messages remain up-to-date and up-to-speed. Leaving the conference I was reminded that sleep quality and mental health are vital aspects of patient management that need to be brought to the table more frequently, and that barriers to conservation need to be broken down, to allow for exchange of ideas and information.
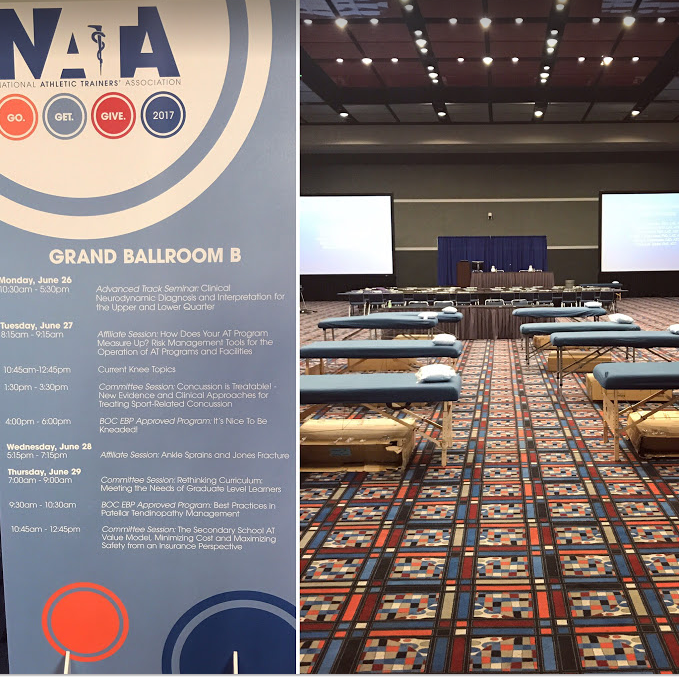
The following day I awoke early to fly to Texas filled with both excitement and unease as we headed towards a conference to present to athletic trainers (ATs) on neurodynamic assessment and treatment. The unease arose from defining our clinical boundaries. Who's role is it to know about pathoneurodynamics, diagnose and prescribe treatments for neurodynamics problems? My initial reaction is that it doesn't belong to ATs. And yet they want to learn. And yet we were there to teach. And the reason I went is because I'm continually reminded that if we don't change the knowledge and practice of those directly working with athletes, how do we change the way athletes are trained, managed and cared for? If we don't break down this profession-specific domain which identifies our roles, how do we make this biggest impact?
As an educator I am reminded that neurodynamics is generally poorly taught and understood. A part of curriculum that is rushed or blazed through to make way for other areas. Yet to be precise, accurate, safe and effective, the study of neurodynamics needs to be presented in a methodical way. The nervous system cannot be delineated from the other systems in our body and therefore teaching neurodynamics needs to be continually presented in a framework that linked back to anatomy, movement and knowledge we know about the neuro-musculoskeletal system. The biggest change we can make is to discuss regressions and progressions of assessment and treatment either side of the standard testing. It was a lot to digest in 6 hours but we did our best to ensure that we presented that framework for clinical neurodynamics and provided a pathway for others to reach continual education materials if they needed.
I finished this weekend feeling encouraged that my current knowledge and clinical practice is shaped by up to-date-research, reminded that without discussion and knowledge sharing the cleft between domains only deepens, and inspired to continue to empower those around me with the information I am given. We need to continue to work towards a collaborate environment where sharing of information is not viewed as making the competition stronger, but rather that sharing of the information allows us to have a greater impact and higher chance of success of achieving what we all set out to achieve. The common goal which drives us all, to help others and to redirect them on the road to recovery.
Everything is connected to everything. Everyone is connected in the same manner as well.
We are all working simultaneously, yet not synchronously, towards the same goals.
I don't for a second think I have all the answers about how to improve the continuum between preventative and rehabilitative care, but I'm confident that if we continue to build this discussion, we'll find our way there.
Sian