Posterior Ankle Impingement - soft tissue
Posterior impingement of the ankle relates to posterior pain on end-range plantarflexion due to compression of posterior bony and soft tissue structures. Although there are many causes for posterior ankle impingement, only soft tissue causes will be addressed here, with bony structures expanded on later.
Posteromedial Impingement
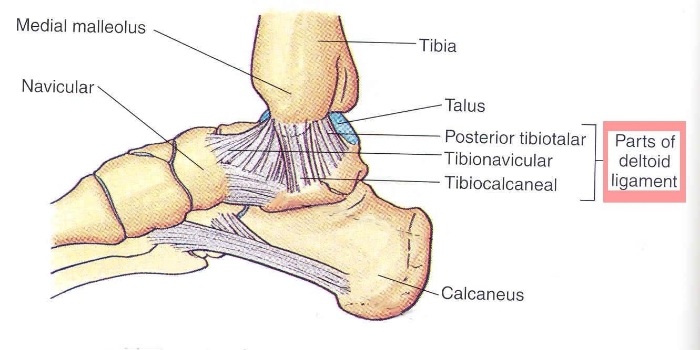
First noted as hypertrophy of scar tissue following a posterior deltoid ligament sprain (Liu & Mirzayan, 1993). Giannini (2013) describes a plantarflexion/inversion sprain as the most common mechanism, with repeated compression of the tibiotalar ligament resulting in secondary hyperplasia and hypertrophic fibrosis (Hess, 2011; Paterson & Brown, 2001). This thickened ligament could potentially irritate the flexor tendons and compress/enclose “posterior tibialis, flexor hallucis longus or flexor digitorum longus” tendons (Giannini et al., 2013).
Clinically, the patient will display localised swelling and TOP at the posteromedial joint line of the ankle. The posterior tibiotalar ligament loses its normal striations and displays some hypertrophy on MRI (Roche et al., 2013), with ultrasound also showing ligamentous abnormalities (Giannini et al., 2013).
Posterolateral Impingement
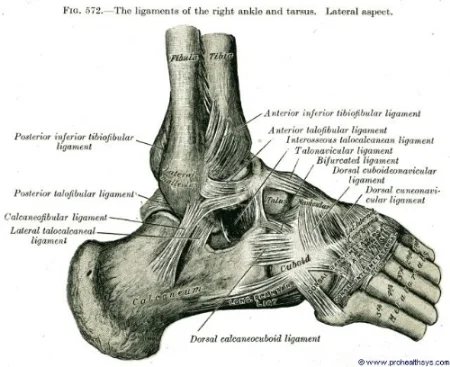
Similarly follows ligament tearing and hypertrophy, involving PTFL and the posterior inferior tibiofibular ligament (PITFL) (Hess, 2011). This causes accessory masses to form which become impinged at end-range plantarflexion; combining with eversion causes further impingement between the distal fibula and the posterolateral border of the talus (Hess, 2011).
Additionally, impingement can occur at the posterior intermalleolar ligament (PIML) with the damaged ligament causing secondary hypertrophy and formation of a meniscoid (Giannini et al., 2013). Repetitive plantarflexion can cause this meniscoid to project into the joint causing locking and pain similar to a knee meniscal injury (Giannini et al., 2013), with forced passive plantarflexion/eversion likely to reproduce pain. MRI is the gold standard, showing a thickened meniscoid posteriorly, with possible bruising of the opposing chondral surface (Roche et al., 2013).
Treatment
Involves both conservative and surgical intervention, with the combination of activity modification and physiotherapy intervention providing good symptomatic relief (Roche et al., 2013). NSAID’s, rest, soft tissue stretches, electrophysical agents, bracing and immobilisation are described in the literature with anecdotal support, showing a 60% success rate in resolving posterior impingement (Giannini et al., 2013; Hess, 2011). While these techniques are offered, there is minimal reference to manual therapy techniques, with only “therapeutic exercises and modalities” (Hess, 2011, p. 296) described with no further elaboration provided.
Maitland (1991) describes two techniques to increase plantarflexion, involving mobilisation of the talocrural joint. If these techniques were performed just before the end-range, increased plantarflexion range, reduced pain and inflammation could be achieved. Given individuals can have asymptomatic bony structures posteriorly (C. N. van Dijk, Lim, Poortman, Strubbe, & Marti, 1995), manual therapy targeting the soft tissue inflammation and increasing the available range of plantarflexion should be sufficient to alleviate symptoms, however further research needs to be conducted to verify this. Corticosteroid and local anaesthetic injections have shown a clinical benefit in reducing pain and improving function in 84% of occurrences (Giannini et al., 2013). The literature also supports a functional rehabilitation program including ankle range and strength exercises, proprioception retraining, sports- specific rehabilitation and taping, in returning an athlete to sport, once all symptoms have settled (Hess, 2011).
If a three to six month conservative program doesn’t resolve symptoms, surgery is indicated, with a posterior ankle arthroscopy the most favoured technique to debride the bony or soft tissue impingement and regain full plantarflexion (C. Niek van Dijk, 2006). Following surgery, a rehabilitation program is initiated at two-weeks post-surgery with estimated return to sport at three months, following a similar program as provided in conservative cases (Hess, 2011).
Alicia
References
** Giannini, S., Buda, R., Mosca, M., Parma, A., & Di Caprio, F. (2013). Posterior ankle impingement. Foot & ankle international. / American Orthopaedic Foot and Ankle Society [and] Swiss Foot and Ankle Society, 34(3), 459-465.
** Hess, G. W. (2011). Ankle impingement syndromes: a review of etiology and related implications. Foot & ankle specialist, 4(5), 290-297.
Liu, S. H., & Mirzayan, R. (1993). Posteromedial ankle impingement. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association, 9(6), 709-711.
Maitland, G. D. (1991). Peripheral manipulation (3rd ed.). London ; Boston: Butterworth-Heinemann.
Paterson, R. S., & Brown, J. N. (2001). The posteromedial impingement lesion of the ankle. A series of six cases. The American journal of sports medicine, 29(5), 550-557.
** Roche, A. J., Calder, J. D. F., & Lloyd Williams, R. (2013). Posterior ankle impingement in dancers and athletes. Foot and ankle clinics, 18(2), 301-318.
Sofka, C. M. (2010). Posterior ankle impingement: clarification and confirmation of the pathoanatomy. HSS journal : the musculoskeletal journal of Hospital for Special Surgery, 6(1), 99-101.
van Dijk, C. N. (2006). Hindfoot endoscopy. Foot and ankle clinics, 11(2), 391-414, vii.
van Dijk, C. N., Lim, L. S., Poortman, A., Strubbe, E. H., & Marti, R. K. (1995). Degenerative joint disease in female ballet dancers. The American journal of sports medicine, 23(3), 295-300.
** - key references