Day 2 Treatment...what now??
A lot of emphasis is placed on a thorough initial assessment, with treatment targeted towards the impairments discovered. But what direction should your treatment take after that initial treatment.
I wrote an earlier blog on The Importance of the Subjective Examination, it is recommended to read that blog first before following up with this post on Day Two Treatment!
Better? Same? Worse?
These questions constantly run through my head during follow-up appointments. If the patient returns better, you can assume your treatment is appropriate and targeting the right areas. If they return worse, you may have underestimated the patient's irritability, however it appears you are treating the right area as your treatment directly affected their presenting pain. If they return the same, maybe your treatment prescription wasn't targeting the right area, maybe you didn't do enough treatment or maybe your initial diagnosis was not correct. This question of "Is the patient better, same or worse?" then directs your follow-up objective assessment and subsequent treatment.
By the end of your initial subjective assessment, you should have a prioritised list of diagnostic hypotheses (e.g. 1. patellofemoral joint pain, 2. fat pad impingement, 3. meniscus injury, 4. knee joint injury etc). This list should also include a prioritised list of contributing factors. In the case of patellofemoral joint pain, a list of factors may include:
PFJ hypomobility
quadricep muscle weakness
hip muscle weakness
ankle dysfunction (hyper/hypomobility)
poor motor patterning (poor single leg squat technique)
lumbar spine dysfunction (hypo/hypermobility, muscular dysfunction, poor motor patterning)
hip joint dysfunction (hypo/hypermobility)
calf and ankle muscle dysfunction
neural dysfunction and many more impairments.
As you can see, it is very challenging to assess all these impairments or contributing factors in one initial assessment. You should assess the most probable factors first, based on your subjective assessment (e.g. PFJ pain - history of ankle injuries, feels like knee rolls in when running - could prioritise hip muscle strength and ankle dysfunction over lumbar spine and neural dysfunction initially).
The list of factors should not be forgotten after the Day 1 assessment, they should be categorically assessed and either cleared/excluded or treated in subsequent treatments.
Asterisk signs (*) are clinical indicators which are measurable, reproducible and relevant to the patient's condition, used as reassessment tools to measure the progress of a patient's condition. They are items that you place an * next to in your notes to highlight the importance of that measure. By the end of your initial consultation, you should have 2-4 subjective asterisks, such as body chart (intermittent shoulder pain, sharp, deep P3-7/10), aggravating factors (running, 10 mins onset P4/10, can continue until 20 mins, P6/10, ceases, takes 3 mins to ease completely), medication use (paracetamol 2x tabs every 6 hours), 24 hour behaviour (presence of P3/10 in AM, eases to P0/10 in 10 mins), functional tasks etc.
You should also have 2-4 objective/physical asterisk signs to reassess within and between treatments. For example, range of motion (right shoulder internal rotation in 90° abduction = 30°), strength (right shoulder external rotation = 3/5), movement diagram (right C4/5 PA half range P4/10 local, no referral), motor patterning (right single leg squat = excessive dynamic knee valgus) etc. You should attempt to have asterisks assessing different aspects of a condition, for example, one asterisk for range of motion, one for strength, one for joint mobility, as your treatment may have effects on different aspects (e.g. joint mobilisations may affect range of motion and strength, or may just affect range of motion).
So by Day 2 (your first follow-up consultation)....you should have a hypothesis list, subjective and physical asterisk signs and a list of impairments/body areas which you still have to assess. The order of your next assessment depends on whether the patient returns better, same or worse?
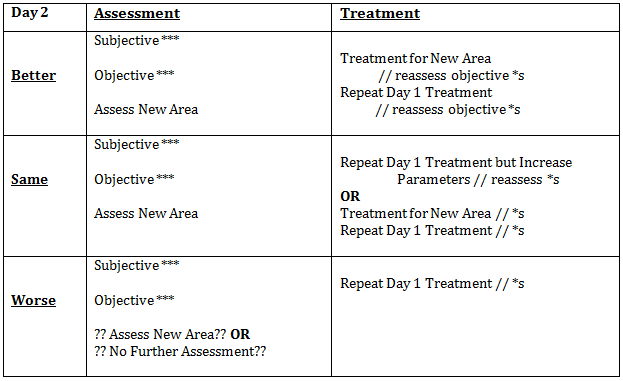
The following table describes the structure I use at each follow-up appointment, which I learnt during our postgraduate study.
Better?
- You question the patient on their subjective asterisks (e.g. "Are you still waking with pain? How long does it take to completely ease?").
- You reassess the physical asterisk signs obtained from your initial assessment (e.g. shoulder internal rotation, strength of external rotation and pain on push-up).
- Then you choose another area to be assessed, which wasn't able to be assessed in the initial consultation, due to time constraints or irritability.
- Once you have completed that assessment, you either decide to treat that area or you exclude that impairment as a contributing factor for the patient's condition.
Same?
- The assessment aspect is the same as if the patient returns better. You reassess subjective and physical asterisk signs then assess a new area.
- The treatment is determined by your findings on the new assessment. If your new assessment appears more relevant than your initial assessment, you can choose to treat that new area, then repeat your Day 1 treatment.
- You must repeat your initial treatment, so you are only changing one parameter each time and can assess your treatment effect. If you add one treatment and remove another treatment you aren't certain if it was the addition or removal of treatments which had an effect.
- If your new assessment excludes that area, you must repeat your Day 1 treatment but increase one parameter, e.g. duration, grade, position.
Worse?
- If the patient returns worse, firstly question them on "how they are worse?" They may have done excessive activity following your treatment or experienced post-treatment soreness, so they appear worse.
- If they are truly worse, you can assume it was your extensive initial assessment which made them worse.
- Firstly, reassess their subjective and physical asterisk signs.
- Then, you repeat the initial treatment.
- If they return for their third consultation worse, you may choose to assess a new area.
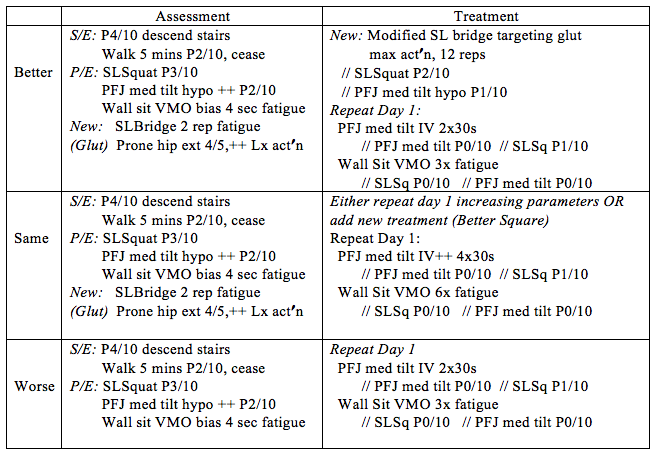
To make it easier to understand...in the case of a standard patellofemoral pain patient...initial assessment findings of tight patellofemoral joint, weak VMO, poor single leg squat technique, nil ligament, meniscal, tendon or fat pad findings. This is a description of the structure I use.
Day 2 Consultation of Patellofemoral Pain Patient.
This seems overwhelming, however the system allows to categorically include and exclude treatments based on efficacy. It increases patient compliance as the patient sees the immediate effect of each intervention. Hopefully this provides you with a framework to follow, which will prevent you "getting bored" and just repeating the same treatment each session. For further information I would recommend consulting the bible for musculoskeletal physiotherapy, Maitland's text listed below.....
Alicia
References:
Maitland, G. D. (1991). Peripheral manipulation (3rd ed.). London ; Boston: Butterworth-Heinemann.
Refshauge, K., & Gass, E. (Eds.). (2004). Musculoskeletal Physiotherapy: Clinical Science and Evidence-Based Practice. Sydney: Butterworth Heinemann.