Shoulder Symptom Modification Procedure - picking the right shoulders to treat
The Shoulder Symptom Modification Procedure (SSMP) was first described by Jeremy Lewis in 2009 and there is a lot of great information available online regarding the performance of this assessment (Richardson & Lewis; Fagkronikk i Fysioterapeuten). The reason I wanted to write about it on this blog is because it ties nicely into the previous three shoulder blogs and offers an alternative assessment procedure and clinical reasoning pathway for shoulder problems. It is not a new approach but one that should be reiterated because maybe like me you hadn't heard it presented in this way?
This process allows for biasing the thoracic spine, scapula and different muscle activation patterns around the shoulder, with each test giving us information and clues to direct treatment and rehabilitation. When I was taught to assess the shoulder originally there was always a focus on structural differentiation. At the time of assessment I tried to identify a painful movement and then see if that pain could be changed by moving the cervical spine, thoracic spine, scapula and muscles around the shoulder. When a change in pain occurred I automatically assumed it was because I had biased one particular structure. After reading Jeremy Lewis' articles and many other papers, I now realise that it is difficult to be so specific about the particular structure you are targeting.
Research has shown and described how the rotator cuff muscles "form a confluent aponeurotic tendon that surrounds the humeral head" (Lewis, 2008, p. 237), which makes it difficult for any single orthopedic test to isolate a particular part of the muscle. From this thinking and knowledge that the diagnostic validity of shoulder orthopedic tests is limited, it became important to still offer an assessment procedure to direct treatment. The focus of the SSMP is to identify movements and techniques that might be contributing factors to the symptomatic movement and not to label the pathology or exact cause of pain. The SSMP also offers a different way to objectively measure the impact of each component on shoulder pain compared to the more traditional special/orthopedic tests.
Image courtesy of Google Images. https://www.londonshoulderclinic.com/wp-content/uploads/2013/03/jeremy-lewis-portrait.jpg
'Dr Jeremy Lewis is a Consultant Physiotherapist, Professor of Musculoskeletal Research, Sonographer and Independent Prescriber. He has been awarded a Fellowship of the Chartered Society of Physiotherapy... and has been acknowledged as one of the 5 most eminent clinicians in his profession. His main areas of clinical expertise are subacromial pain (impingement) syndrome, rotator cuff tendon problems, shoulder pain syndromes and frozen shoulder.' (London Shoulder Clinic, 2015).
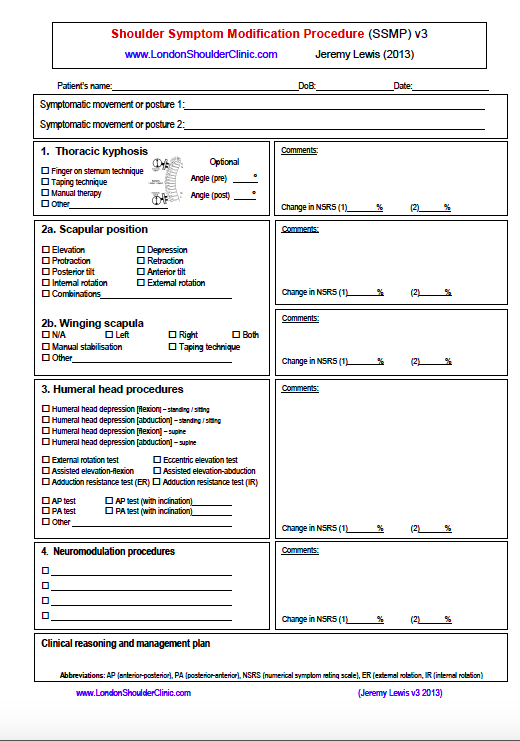
The Shoulder Symptom Modification Procedure is available through the London Shoulder Clinic. As you will see there is time dedicated during the assessment to look at the impact of the thoracic spine, scapula positioning, humeral head position, and other neuromodulation techniques on shoulder pain. Lewis & colleagues (2015) go through this assessment in great detail and I would highly recommend reading the original article.
The first step is to identify 1-3 symptomatic movements for the assessment. Determining whether the changes are clinically significant relies heavily on the impression of the patient and how they feel during the test. It is important to explain to the patient prior to assessment that their feedback and participation is crucial to help guide the treatment pathway.
- The first focus is the impact of thoracic spine posture. Depending on the functional demands on the patient, you may be able to use postural correction or you may need to tape the thoracic spine to maintain a particular position during the symptomatic movement. If pain is improved 100% in this stage, the assessment is ceased and treatment begins.
- The second component is the scapula and in this stage the clinician alters the starting position of the scapula based on their assessment, and then the patient moves independently through their symptomatic movement. The corrected starting position might involve more than one movement.
- If symptoms are not improved with scapula repositioning then the next focus is on positioning of the humeral head. One example is the external rotation test which uses theraband resistance into external rotation during active shoulder flexion and is performed independently by the patient. As you can see on the form below there are many tests within the humeral head section and your assessment is likely to be directed by the symptomatic movement.
- The final component involves neuromodulation techniques, which may include manual therapy techniques for the cervical or thoracic spine or soft tissue treatment of the muscles around the shoulder. These techniques are used if the first three stages don't produce a significant change in symptoms.
In this video Chris Lendrum and Glen go through their approach to using this procedure and offer handing positions for each test. It doesn't cover every step of the procedure but helps visualise how this assessment is put into practice.
The benefits of using the approach in your assessment of shoulders is that it helps us to understand the impact we might have on pain and function and it gives immediate direction for treatment, often referred to as a 'green light'. While the reliability and validity of this procedure remains to be determined, it offers an alternative method for objectively assessing the shoulder (Lewis et al., 2015) and in my opinion, in many ways offers more direction for treatment that the traditional shoulder tests.
One thing that is very powerful about using the SSMP is showing your patient how exercises/treatment can help. I am a big believer that we need to prove that treatments work before we implement them. For manual therapy techniques I often perform a mini treatment to explore the impact a treatment technique has before performing the full dosage. This helps with patient compliance, my clinical reasoning and showing patients that you are only doing what you can show works. The same thought process applies for the shoulder, except it is often really tricky to make immediate change and rehabilitation can be lengthy. Being able to show patients why they need to perform a certain exercise by producing immediate changes in their pain will motivate them to persist with their independent exercise program and give them hope for their recovery.
Conclusion
When I went through Masters I seemed to gain bits and pieces of approaches and different techniques for assessment and treatment, without fully understanding each in detail and knowing when to use them. After researching these shoulder blogs I have come to realise that there are distinct schools of thought and many Physiotherapists currently researching different aspects of the shoulder. Now I see that I was taught aspects of Jeremy Lewis' approach and my teachers at the time called it structural differentiation (which is not entirely correct). I was taught about the importance of scapula upward rotation without being introduced to the ideas of Lyn Watson. I was reminded the importance of viewing the shoulder as one component within the kinetic chain, something that has been extensively researched by Ben Kibler. And, I was given techniques for individually assessing and strengthening muscles around the shoulder responsible for scapula control, without understanding the in-depth research that Physiotherapists like Anne Cools have conducted. In reality, it is likely that clinicians will draw on all of these approaches to select the best assessment procedure and treatment pathway for their patient. Putting it all together makes the process much clearer, which is encouraging considering how complicated shoulders can be. It has been an enjoyable and insightful journey to learn about the techniques which were passed onto me by teachers in my career. I hope you too now have a broader perspective and at the end of this blog, can recognise different approaches, understand more about the backgrounds of each, and appropriately implement them into your clinical practice.
Sian
If you'd love to listen more about the perspective of Jeremy Lewis, there is a podcast available on Sound Cloud through Physio Edge relating to the management of Frozen shoulder.
References:
Lewis, J. S. (2008). Rotator cuff tendinopathy: A review. British journal of sports medicine.
Lewis, J., McCreesh, K., Roy, J. S., & Ginn, K. (2015). Rotator Cuff Tendinopathy: Navigating the Diagnosis-Management Conundrum. The Journal of orthopaedic and sports physical therapy, 1-43.