APA 2017 Momentum Conference Lumbopelvic Summary
Three weeks ago, I attended the Australia Physiotherapy Association Momentum 2017 conference in Sydney. It was my first time attending a conference, and it was amazing! I expected to feel brain-dead and be sick of research and statistics by the end of the conference. Instead, I learnt something from every presentation, caught up with a lot of colleagues and friends, and challenged my current understanding of physiotherapy.
So I thought I would give a summary of my conference, the interesting tid-bits I learnt, or journal articles which piqued my interest...
1) Low Back Pain
Tim Mitchell, Specialist Musculoskeletal Physio
Tim Mitchell
A Clinical Framework for Identifying Modifiable & Non-modifiable Contributors to Disabling Low Back Pain
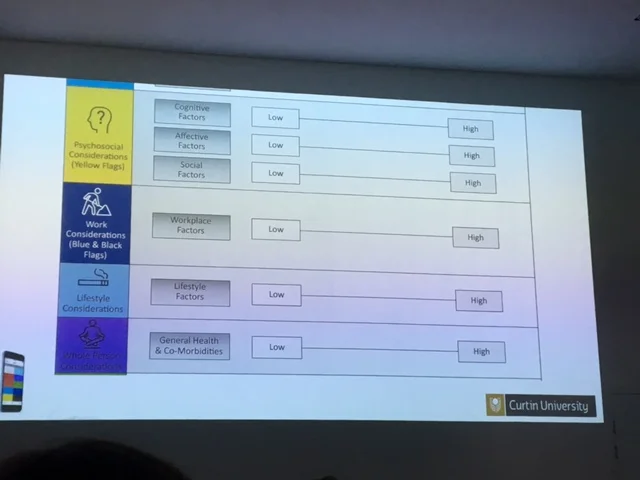
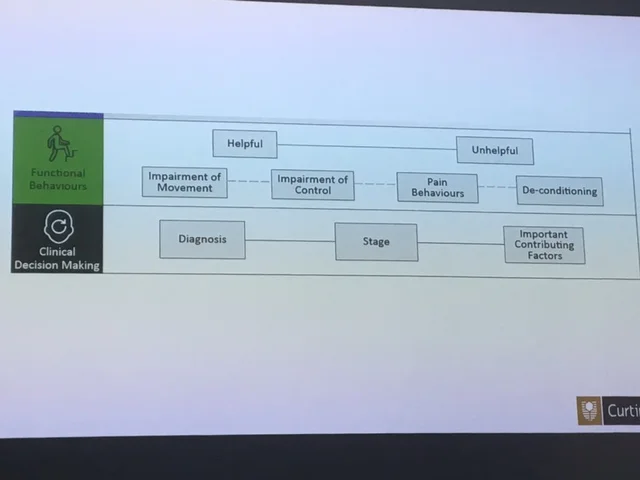
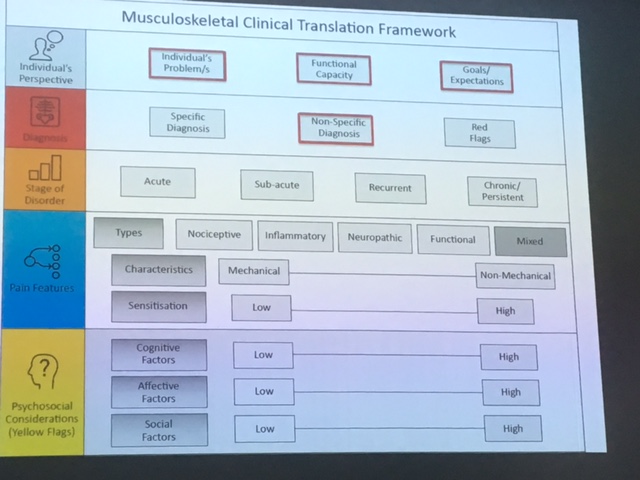
Tim works at Curtin University with Darren Beales, Peter O'Sullivan and Helen Slater, coordinating and presenting on the undergraduate and Masters physiotherapy programs. They have developed a framework to "demystify" the lumbar spine, effectively summing up all aspects of assessing and managing a lumbar spine injury.
It is continuing to be updated, with feedback from clinicians, so feel free to critique the framework. I believe the framework provides a lovely base to then work from, especially in your first 10 years of physiotherapy. It addresses joint factors, movement patterning impairments, psychological contributors, motivations and barriers to recovery.
The framework is available for purchase on iBooks, titled Musculoskeletal Clinical Translation Framework, by Tim Mitchell, Darren Beales, Helen Slater and Peter O'Sullivan, for $19.99 with proceeds donated back to Curtin University physiotherapy program. The framework gives clinical examples and case studies to work through, using the framework. For those undergoing, or planning on undertaking, Masters post-graduate studies, this would be a great resource.
Images courtesy of Tim Mitchell, APA 2017
Peter O'Sullivan, Specialist Musculoskeletal Physiotherapist
Peter O'Sullivan
Cognitive Functional Therapy for Disabling Low Back Pain
Peter followed Tim, discussing the cognitive functional therapy model which Peter developed to treat low back pain.
I have had many discussions in the past few years about Peter's approach to treating lumbar pain. To clarify, Peter is a manual therapist, he puts his hands on every patient he assesses and treats. However, due to Peter's skill set and reputation, he sees predominantly chronic low back pain patients with pain lasting at least 6 months who haven't responded to manual therapy with previous therapists. His clientele often aren't appropriate for extensive manual therapy, as this hasn't been effective, however Peter will always put his hands on the patient to assess muscle tone, muscle activation, joint mobility etc.
There is the tendency to assume that Peter utilises exercise therapy with every patient, and avoids manual therapy, however again this is appropriate to his clientele. The cognitive functional therapy approach includes manual therapy, exercise therapy, education, psychology and referral for additional services if required, addressing the individual aspects of a patient's condition, individualised to each patient. The moral of the story is assess the patient's mobility, motor patterning, habits, behaviours and then address them, using a multi-faceted program, relevant to each individual patient.
So after all that, what did Peter actually talk about at the conference?
"Context"
- Peter used this word to describe the cumulative factors that sensitise a patient's pain system
- This could include poor sleep, increased work hours, stressful life events (moving house, death in family), increased training load, illness (ongoing cold symptoms), reduced exercise/meditation
- Individually each situation is a stressor, but the cumulative effect or "context" can have much greater implications on their pain system
"Strong therapeutic alliance"
- The role of the physiotherapist is to form a team with the patient
- The therapist should facilitate however the patient should be an active member of their rehabilitation
- Treatment/management should consist of techniques aimed at making the patient independent and able to self-manage, not rely on the therapist for regular passive intervention
"Decrease sympathetic wind-up"
- Desensitise the painful region with pain-free exposure
- Manual therapy and exercise prescription should be used to reduce local pain, to then allow pain-free movement
- You must then integrate these new behaviours into previously painful movements, to develop new memories and reduce fear
- e.g. squatting brings on multisegmental lumbar pain, as the patient maintains lumbar hyperextension throughout the movement, treatment to regain lumbar flexion (e.g. lumbar muscle release in sidelying progressing into greater hip/lumbar flexion, anterior/posterior lumbar mobilisations, lumbar flexion physiological mobilisation, diaphragmatic breathing in Child's pose position etc) must be followed with retraining the squatting technique out of hyperextension
- By reinforcing a pain-free squat with new technique, after desensitising the local painful tissue, the patient forms new memories of squatting and breaking old habits
For more information on Peter's Cognitive Functional Therapy approach to treating lumbar pain, the following articles are excellent!
O'Sullivan 2015, in Physical Therapy 95:11
Bunzli 2016, in Physical Therapy 96:9
Vibe Fersum 2013, in European Journal of Pain 17
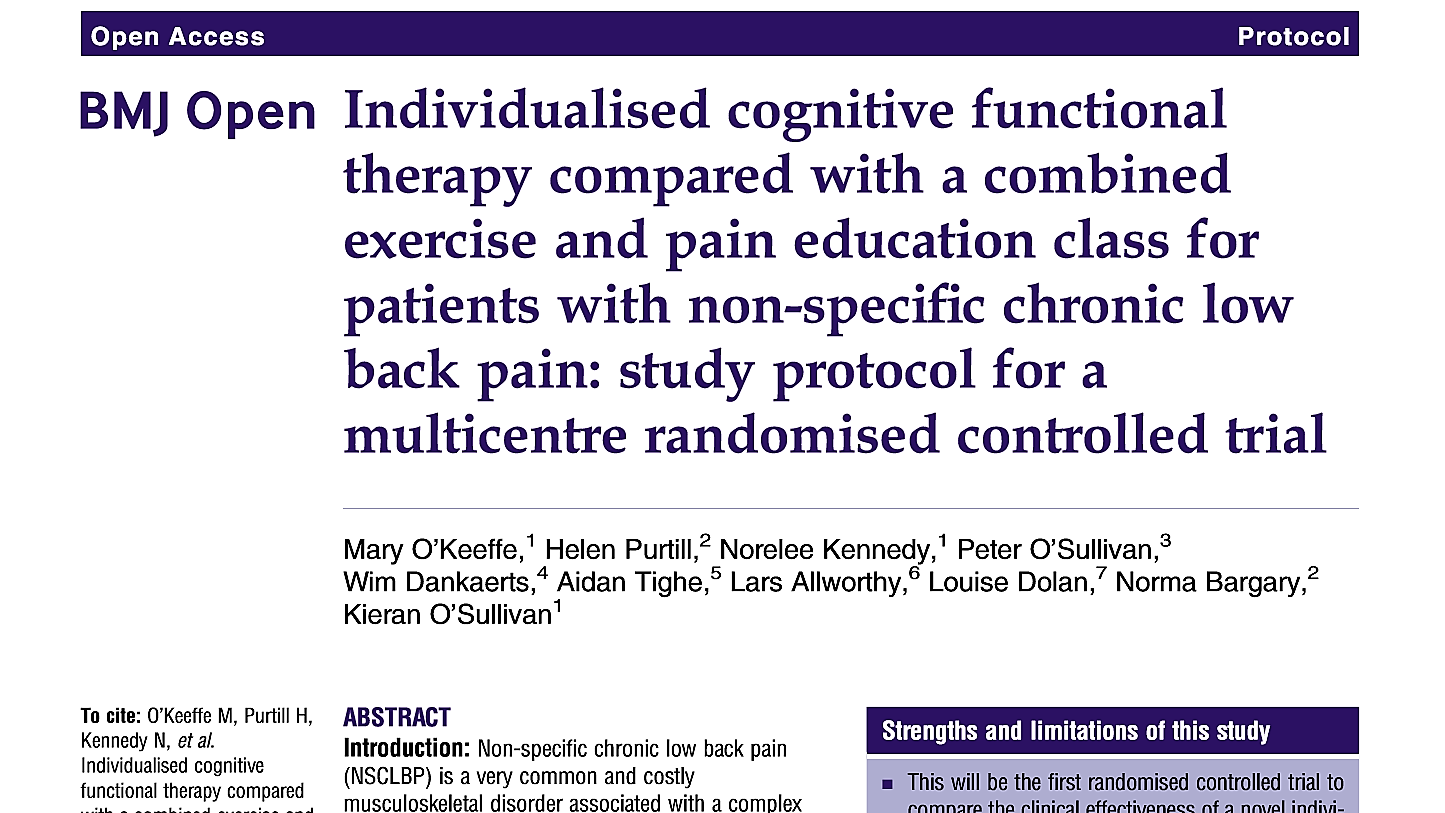
O'Keeffe 2015, in British Medical Journal 5
Darren Beales, Specialist Musculoskeletal Physiotherapist
2) Pelvic Girdle Pain
Darren Beales
The Influence of Pain & Other Factors on Motor Function
Following in the Curtin University vein, Darren Beales is world-renowned for his articles on Pelvic Girdle Pain in 2009, with Peter O'Sullivan. He presented on pain causing motor patterning issues and altered muscle function, rather than motor patterning and altered muscle function causing pain.
Darren discussed the recent study by Helen Slater and colleagues (2016), which found females tested at 20 and 22 years of age, who reported severe menstrual pain had heightened sensitivity to cold (at an area distant to their menstrual pain region) and heightened pressure sensitivity (at the area of menstrual pain). This suggests those who report higher menstrual pain have altered central and peripheral neurophysiological processing, giving greater pain sensitivity.
Paananen, in 2015, utilising the same Raine Study (a Western Australian pregnancy cohort study following females from birth) found those females with low cortisol levels in response to stress, had greater musculoskeletal pain levels. Those with combined lower cortisol levels and lower thresholds on pressure testing had even higher pain levels.
Another study by Palsson (2015) looked at tissue sensitivity in pregnant females. They compared pregnant females to non-pregnant female controls, assessing sensitivity to light touch, pin-prick and pressure testing, along with active straight leg raise (ASLR) and SIJ pain provocation tests. They also completed questionnaires regarding sleep, wellbeing and disability. The pregnant females were divided into high or low pain groups, with the high pain group reporting greater difficulty on ASLR and both pregnant groups reporting greater pain on provocation testing. Both pregnant groups reported much lower pain pressure thresholds (pressure became painful at a much lower level than those non-pregnant). Those in the high pain group had poorer sleep and wellbeing than the low pain group, but there was no difference between pressure thresholds and disability.
So if all pregnant females have a sensitised pain system, but those with higher pain levels have poorer sleep and wellbeing, should we try address sleep and stress levels, rather than motor control?
Should the ASLR only be used as a reassessment tool, to determine which strategies improve heaviness, rather than just as a positive/negative test (see Sian's previous ASLR post)?
Active Straight Leg Raise (ASLR)
ASLR - with oblique abdominal activation
ASLR - with pelvic compression
Beales (2016) found those with persistent pregnancy-related pelvic girdle pain post-partum had higher levels of kinesiophobia, altered body perception, poor sleep quality and poor sleep adequacy, compared to those with no pain post-pregnancy. This gives moderate disability, similar to levels experienced by those suffering from chronic low back pain. It suggests sleep quality and quantity, fear avoidance and body perception should be assessed, and managed, when treating those with persistent pelvic girdle pain, following pregnancy.
Palsson (2015) also completed a study where they injected saline into the long posterior sacroiliac ligament, with VAS pain levels, pressure pain thresholds, difficulty on ASLR and EMG levels of the trunk and thigh muscles. Compared to baseline levels and control group, those injected with hypertonic (pain-inducing) saline had higher pain levels, reduced tolerance to pressure, increased difficulty performing the ASLR and a bilateral increase in trunk and thigh muscles. This suggests that pain in the SIJ region causes secondary biomechanical changes in the lumbopelvic region, rather than biomechanical changes causing SIJ pain.
Does our management need to be targeted towards addressing pain to improve motor control, rather than addressing motor control to reduce pain?
In conclusion, Darren reported the need to:
- address nervous system sensitivity in pregnancy, regardless of their pain levels
- educate the patient so they can understand and feel empowered, rather than helpless
- address their breathing pattern, avoid breath holding & erratic breathing (to desensitise the pain system & reduce stress response)
- promote normal, relaxed movement
- improve body awareness & proprioception
- integrate into functional, whole body movements
- provide conditioning training, to utilise the global effects of exercise therapy
These presentations both reinforced and challenged my current thinking of lumbar and pelvic conditions. Hopefully, this continues to improve your management of these injuries!
The next blog will focus on gluteal tendinopathy and rotator cuff tendinopathy issues.
Alicia
References:
Beales, D., Lutz, A., Thompson, J., Wand, B. M., & O'Sullivan, P. (2016). Disturbed body perception, reduced sleep, and kinesiophobia in subjects with pregnancy-related persistent lumbopelvic pain and moderate levels of disability: An exploratory study. Manual Therapy, 21, 69-75.
Bunzli, S., McEvoy, S., Dankaerts, W., O'Sullivan, P., & O'Sullivan, K. (2016). Patient Perspectives on Participation in Cognitive Functional Therapy for Chronic Low Back Pain. Physical Therapy, 96(9), 1397-1407.
Fersum, K. V., O'Sullivan, P., Skouen, J. S., Smith, A., & Kvale, A. (2013). Efficacy of classification-based cognitive functional therapy in patients with non-specific chronic low back pain: A randomized controlled trial. European Journal of Pain, 17(6), 916-928.
Hodges, P. W., & Smeets, R. J. (2015). Interaction Between Pain, Movement, and Physical Activity Short-term Benefits, Long-term Consequences, and Targets for Treatment. Clinical Journal of Pain, 31(2), 97-107.
O'Keeffe, M., Purtill, H., Kennedy, N., O'Sullivan, P., Dankaerts, W., Tighe, A., . . . O'Sullivan, K. (2015). Individualised cognitive functional therapy compared with a combined exercise and pain education class for patients with non-specific chronic low back pain: study protocol for a multicentre randomised controlled trial. Bmj Open, 5(6).
O'Sullivan, K., Dankaerts, W., O'Sullivan, L., & O'Sullivan, P. B. (2015). Cognitive Functional Therapy for Disabling Nonspecific Chronic Low Back Pain: Multiple Case-Cohort Study. Physical Therapy, 95(11), 1478-1488.
Paananen, M., O'Sullivan, P., Straker, L., Beales, D., Coenen, P., Karppinen, J., . . . Smith, A. (2015). A low cortisol response to stress is associated with musculoskeletal pain combined with increased pain sensitivity in young adults: a longitudinal cohort study. Arthritis Research & Therapy, 17.
Palsson, T. S., Beales, D., Slater, H., O'Sullivan, P., & Graven-Nielsen, T. (2015). Pregnancy Is Characterized by Widespread Deep-Tissue Hypersensitivity Independent of Lumbopelvic Pain Intensity, a Facilitated Response to Manual Orthopedic Tests, and Poorer Self-Reported Health. Journal of Pain, 16(3), 270-282.
Slater, H., Paananen, M., Smith, A. J., O'Sullivan, P., Briggs, A. M., Hickey, M., . . . Beales, D. (2015). Heightened cold pain and pressure pain sensitivity in young female adults with moderate-to-severe menstrual pain. Pain, 156(12), 2468-2478.