Outside the Orthopaedic Protocol
This week we welcome Physical Therapist, Michael McGowan (DPT) to share with Rayner and Smale a unique case study about a complex combination of orthopaedics and oncology. I met Michael through the growing network of Physical Therapists writing online and sharing their personal experiences with our profession. Michael graduated from Springfield College in 2016 and currently works as a physical therapist in a hospital-based outpatient clinic in Hartford, CT treating a diverse patient population with both neurological and orthopaedic diagnoses. Michael's main interests and motives revolve around improving patient-centered care unlike many graduates who are solely knowledge hungry for clinical tips about treatment strategies and 'tricks'.
We don't work in the healthcare business managing people. We work in the people-managing business offering healthcare. It's not an easy job and we don't chat enough about the emotional impact physical therapy has on our lives. Michael shares his perspectives about the more philosophical side of our profession on his blog thelittlethingsinpt, which I really enjoy reading. So I am excited to share the experience of a fellow PT who loves to challenge and reflect on the way we manage people.
Introducing Mrs. P
Mrs. P is a 58 year old woman who presented to hospital after falling in her driveway in September 2016. Upon admission, X-rays and scans were ordered which ultimately revealed an osteosarcoma on the distal end of the left femur, which had also spread diffusely throughout the distal aspect of the left lower extremity.
Following the diagnosis of a largely spread osteosarcoma, directly affecting the structural integrity of the bone, the patient was managed with an ORIF (open reduction internal fixation) of the left distal fibula, a complex left Total Knee Arthroplasty (TKA), all concurrently following radical resection of the distal left femur to remove any cancer remaining. This procedure is unique to the region of Hartford, where a talented surgeon specializes in orthopaedic oncology cases, otherwise noted as Extreme Orthopaedics. Often times, patients who see this specialist have tried other options primarily and are looking for a second opinion, or, more often than not, as in this case, the scenario is too complex for a typical orthopaedic surgeon, so the specialist is then called upon. Another unique aspect of Extreme Orthopaedics is that there is often is no protocol for rehabilitation. The patient typically presents to physical therapy as weight bearing as tolerated, but other than that, the surgeon leaves it up to the therapist’s discretion for the rest, with the ultimate goal of getting back to function as quickly, but as safely, as possible. Fortunately for us as physical therapists, the surgeon has confidence to allow us the autonomy over directing the patient’s care.
Back to the case. This patient undergoing a 3-part surgery not only is unusual as compared to a typical post-operative orthopaedic patient, but the combination of the distal fibular ORIF, TKA, as well as resection of the distal femur resulted in pain, loss of function, significantly decreased range of motion, and decreased strength. Furthermore, when an orthopaedic case arises, at times, surgeon’s will likely address one condition as the priority and return for future procedures to prevent an extended recovery. However, in cases like this, when it was adamant to resect the cancerous infiltrates on the bone, these three procedures needed to be combined at all cost of patient function.
Mrs. P’s plan of care ended in April 2017, as she had returned to highest potential of premorbid function prior to her fall, terminated all chemotherapy treatments, returned to work as sales consultant working from home, as well a regained baseline normative values in regards to strength and range of motion bilaterally throughout the lower extremity joints.
While current cancer treatment “may improve survival, the side effect on physical and psychological function often reduce quality of life. There is an increasing need for rehabilitation to address these issues” (Dennett, et al., 2016, p.68). Of all the hardships this patient underwent during her plan of care beginning in October 2016, nothing had more of a negative impact on rehabilitation than the chemotherapy treatments. The patient received these treatments a month from beginning physical therapy, and with cycles occurring monthly, the patient suffered from significant adverse effects that are typically seen with chemotherapy. On the contrary to what I originally believed, it is not the first day or two after chemotherapy that drains the patient, the devastating effects did not set in until 3 or so days after treatment for this patient. Granger (2016, p.61) found that in lung cancer patients, the side effects of cancer treatment involving 'bone marrow suppression and resultant immunosuppression, are worst two weeks following treatment'.
For Mrs. P, dehydration, fatigue, nausea, weakness, and depression caused difficulty keeping up with the timeline in which had originally been set. These side-effects were not only caused by the chemotherapy treatments, but also due to the secondary effects of the powerful intervention targeting not only the cancerous cells, but all of the cells of the body. This is why the patient would frequently attend visits to the oncologist prior to therapy visits to either receive a blood transfusion or fluids as the treatments acted most by depleting the total blood count. With the heavy symptomatic response, this left a very small window to achieve the outcomes and increase intensity of activity appropriately prior to the next cycle beginning again. There is a continual challenge to understand how and when physical therapy can benefit a patient who is receiving chemotherapy treatment. Not only do the patient's feel unwell (as described above) but their bodies are severely impacted on a cellular level which changes their ability and response to physical load.
On a global level, we all know that a sedentary lifestyle does not improve our health, so we can't allow for us to change our perspective on the benefits of exercise following the diagnosis of cancer. What we can change is our expectations on what type of physical activity we teach and promote (Newton & Galvao., 2008). Our role to promote and prescribe exercise should also involve educating the patient about the benefits of physical activity and how it can impact the ultimate prognosis in a positive manner.
Following diagnostic procedures confirming cancer, for example, a PET scan, exercise can have positive benefits on managing chemotherapy and radiation treatments. These benefits consist of, but not limited to improving psychological health, improving strength and flexibility, reducing depression, maintaining overall levels of function, and increasing cardiovascular health and fitness with correct implementation of exercise prescription. Exercise is also shown to increase survivorship post cancer diagnosis as well as improve overall immune function, which is a significant implication with chemotherapy, as chemo is known to wipe out immune system significantly (Newton & Galvao., 2008).
It can be difficult to prescribe a set amount of exercise as the patients are most likely going to encounter good and bad days. Cancer-related fatigue can be most detrimental side-effect of the disease and of their treatment. What is encouraging to know however, is that exercise helps to actually decrease effects of fatigue, whereas rest actually heightens fatigue further (Dennett, et al., 2016; Newton & Galvao., 2008). In 2016, Dennett and colleagues conducted a systematic review to investigate the dose-effect response of exercise on cancer-related fatigue to understand further how much exercise is safe for an immuno-compromised individual. There results were positive and the take hope messages were that exercise does reduce fatigue, it is safe with low risk of side effects and does not negatively impact inflammatory markers in the blood. The one precaution stated in this article was that high intensity exercises for long periods can result in immuno-suppression in this patient population and clinicians need to carefully prescribe exercise dosage based on the patient they are treating. Their study also showed that these positive impacts are more readily seen in cancer patients with solid tumours but less in haematological cancers.
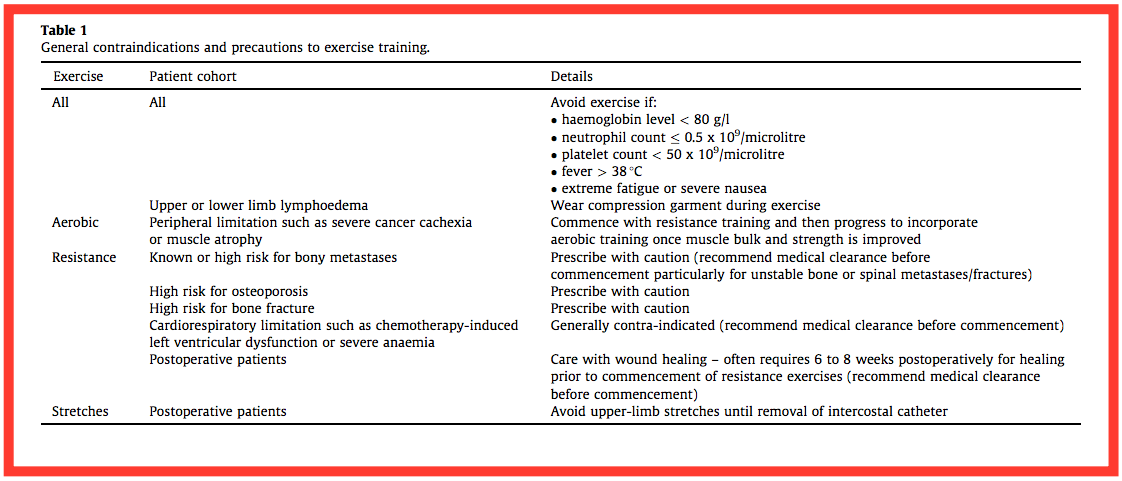
Below is a table describing the contraindications for exercise in cancer patients (Granger, et al., 2016, p. 64).
“Despite these benefits of exercise, there is a lack of evidence on the safety and efficacy of exercise in relation to dose. The ideal mode and intensity of exercise for people with cancer is unclear, and exercise guidelines are based largely on expert clinical opinion and adaptations of guidelines for healthy people.” (Dennett, et al., 2016, p.68). Here are the current guidelines for exercise prescription for patients diagnosed with cancer (Dennett, et al., 2016; Newton & Galvao., 2008):
- Aerobic exercise 20-60 minutes, 3-5 times per week at 55-90% max HR (physical therapist can help patient determine this level).
- Resistance exercise consisting of 6-12 repetitions, repeated for 1-4 sets for major muscle groups 3 times per week. If fatigue is a barrier to participation, resistance exercises are often the best option for patients, as they are intermittent in nature with incorporated breaks between sets, as well as come with a lower cardiovascular demand when compared to endurance/aerobic exercises.
- Flexibility activities 2-4 sets, 2-3 times per week.
- Dennett et al (2016) found that the greatest benefits occur with a combination of aerobic and resistance exercise.
- ** Ranges seen (e.g. 20-60 minutes) are wide and diverse, demonstrating the inconsistencies with research in patients with cancer. Conclusive on the benefits, but still inconclusive on EXACT prescription.
However, like any guideline, these must be interpreted on a patient by patient basis, rather than solely basing it off the cancer diagnosis. The patient should be able to respond to each activity with appropriate levels of fatigue and other exercise related changes. Additionally, the exercise habits and tolerance prior to diagnosis will also have an impact on overall exercise prescription as well.
MANAGING THE EDGE CASE PATIENT
The primary area of pain was the knee, rightfully so. This pain was variable in nature with a continuous achy and intermittent sharp pain. The patient described this as a diffuse aching over the anterior aspect of the knee and the intermittent pain running proximally over the anterior thigh. The patient rarely expressed symptoms regarding the foot and ankle during treatment, however. Although, she responded exceptionally to a home exercise program regarding her right ankle in order to maintain, if not further progress, the function of her ankle.
Upon evaluation, the patient demonstrated:
- A lack of hip flexion, extension, and abduction strength and range of motion.
- A decrease in knee flexion with intense pain upon > 90 degrees of flexion.
- Limited ankle mobility restricted by pain.
- Other measures for strength and range of motion were within normal limits throughout the right lower extremity.
- The impairments above resulted in an altered gait presenting as a favoring of the right lower extremity even using a straight cane. The consequence of this compensation was a weight shift of the trunk away from the left lower limb.
- Other compensation patterns were present such as a quad-dominant squat pattern driven by a fear of falling backwards when placed on heels during posterior weight shift.
Functional limitations beyond decreased muscular strength, proprioceptive capabilities, and decreased functional movement pattern ability, was the reduced cardiovascular tolerance and endurance. This placed a barrier to the frequency and intensity of treatment which was required for return to premorbid levels of strength.
This case was of particular interest to me because of the complex system interactions between neurology, oncology and orthopaedic conditions, not to mention the psychological and emotional impact this single event of falling had on Mrs. P’s life. It is one thing to fall and break a hip and another completely to fall, break several bones and be diagnosed with widespread cancer. There are times when it is inconceivable to understand what patients have gone through before they come into our lives, to sympathize with their loss, to be their coach and cheerleader and to rationally work towards providing them with the pathway to optimal recovery. I remember learning about chemotherapy during my training and it was a great learning experience to understand how chemotherapy truly impacts someone’s physical well being.
Aside from weakness and altered function, one of the hardest challenges we faced was the impact and side effects that the chemotherapy treatment had on this patient, with regards to tolerance to treatment. This side effects lasted up to a week following the 2-3 day dormant period following treatment. At times, the patient presented with very low blood pressure < 90/60 mmHg, with an elevated resting heart rate which did not seem appropriate to challenge the cardiovascular system extensively. With such rare conditions we need to take a step-by-step approach and this needs to be communicated with our patients. I definitely did not know all the answers to begin with or have a clear vision of what to predict. In each step of the treatment I relied on patient response to treatment, vital signs, as well as appropriate progression of exercises and activities in order to meet the appropriate demands of the system without over-challenging. Additionally, referring to evidence in the literature played a large factor in ensuring proper progression without over-exertion. In order to make the best decisions about the plan of care, I also used knowledge in regards to previous patients I or a co-worker had treated undergoing the treacherous effects of chemotherapy. This brought me back immediately to my clinical medicine based thinking about oncology and exercise learned back in school, as well as my clinical knowledge of treatment prescription to adequately challenge the patient.
MAINTAINING AN OPEN LINE OF COMMUNICATION.
A key focus of Mrs. P’s management was communication and establishment of rapport. There was a constant balance that needed to be met between presenting as a confident therapist, providing sympathy and understanding, educating Mrs. P about the risk/rewards for continuing with treatment and exercise, and providing an environment to discuss her thoughts and perspectives. There was also the issue of dependency, in which the patient even admitted that it was scary to think of going on week by week without the guidance of a physical therapist after working together for the past 7 months. Not only did the patient receive assistance on a physical level, but through compassion and just being a listening ear, the patient seemed to develop a deeper trust in conjunction with the traditional patient rapport that the therapist had hoped to achieve. The line of communication was opened but to the point where restoration of confidence must be preached in order to return to premorbid way of life.
A commendable trait that Mrs. P possessed was honesty. Her communication was always honest and this helped to build trust between myself as the therapist and the patient. The patient was always true to their symptoms, and vital signs seemed to always align with symptoms being expressed. Mrs. P never used a lie to get out of therapy and battled nausea, sickness, and other effects of chemotherapy during plan of care that were handled appropriately by the therapist and patient. The patient was able to translate and relay information stated upon monthly visits with the orthopedic/oncology surgeon which aligned consistent with the notes that were accessible in the computer documentation system.
A third aspect of communication pertinent to this case study was maintaining contact with surgeon to monitor patient progress, discuss PT and allow for patient review for any oncology signs. The surgeon was receptive to physical therapy feedback, always seemed to be in agreement with plan of care, and supplemented PT support by advocating for rehabilitation in order to return to highest possible function. Another confirmation of how important and adamant it is to not be fearful of communicating with physicians, as their perspective and knowledge only allows for growth and development into your plan of care for the patient.
CONCLUSION
Managing both musculoskeletal pain, orthopaedic conditions and cancer rehabilitation places a large demand on the therapist to use clinical reasoning to guide rehabilitation and predict recovery outcomes. Many of the orthopaedic protocols we implement as PT’s are developed for low complexity cases. This was not considered a black and white case. It fell in the very grey area in which as new graduate, I had to take my treatments step by step in order to understand what it was that the patient needed most from therapy and what our treatment goals would be. This case was a reminder of the need to not only consider the patient’s within the biopsychosocial framework but to truly focus on the person that is in front of us, not the condition they bring with them. At the end of the day, we are just people doing our best to help other people, and if we stop seeing them as those people and just label them with a diagnosis, we will lose touch with what we love.
Michael McGowan
REFERENCES
Dennett, A. M., Peiris, C. L., Shields, N., Prendergast, L. A., & Taylor, N. F. (2016). Moderate-intensity exercise reduces fatigue and improves mobility in cancer survivors: a systematic review and meta-regression. Journal of physiotherapy, 62(2), 68-82.
Granger, C. L. (2016). Physiotherapy management of lung cancer. Journal of physiotherapy, 62(2), 60-67.
Newton, R. U., & Galvão, D. A. (2008). Exercise in prevention and management of cancer. Current treatment options in oncology, 9(2), 135-146.