Can the risk of Vertebral Artery Dissection be determined with pre-manipulative screening?
Cervical manipulation has inherent risks. One of the the most dangerous adverse effects following cervical manipulation is vertebral artery dissection (VAD) and stroke. “The frequency of stroke in the vertebral and basilar arteries territory is highly variable ... ranging from 0.2 to 50 cases per one million manipulations” (Tinel et al., 2008, p. 404). For the past two decades, functional pre-manipulative screening tests have been used by Physiotherapists to identify patients at risk of vertebrobasilar insufficiency (VBI).
Many experts in the field of VAD and cervical manipulation have started to question the clinical validity and diagnostic utility of these tests. Currently there is great uncertainty if the tests themselves are potentially dangerous enough to cause VAD. In response to this current research, clinical guidelines have changed to place a greater emphasis on subjective examination of a patient presenting with neck pain, headache, and dizziness. This now involves more thorough questioning of medical and general health, identification of thrombolytic risk factors and markers of cardiovascular disease, and identification of red flags associated with hind-brain ischemia. As research continues to evaluate the cause of VAD and determine correlation between this and cervical manipulation, therapists need to remain aware that while the risk is quite small, our ability to determine the safety of manipulation is not flawless. Medical imaging is being used more frequently to assess the integrity of the cervical spine with XRAY and the integrity of the vertebral arteries with Doppler US.
Previously I knew that there was controversy about wether you should perform the pre-manipulative testing or not, but I didn't know why this was the case. This blog aims to review the risks of cervical manipulation, the clinical presentation of VBI and the current assessment recommended by the Australian Physiotherapy Association. I'm also pleased to include the thoughts and recommendations of Dr. Mark Percy, Specialist Radiologist from MIA Lilydale, Victoria. Dr. Percy shares the recommendations and concerns from a Radiologist's perspective.
mechanism of injury of Vertebrobasilar insufficiency & risk of cervical manipulation
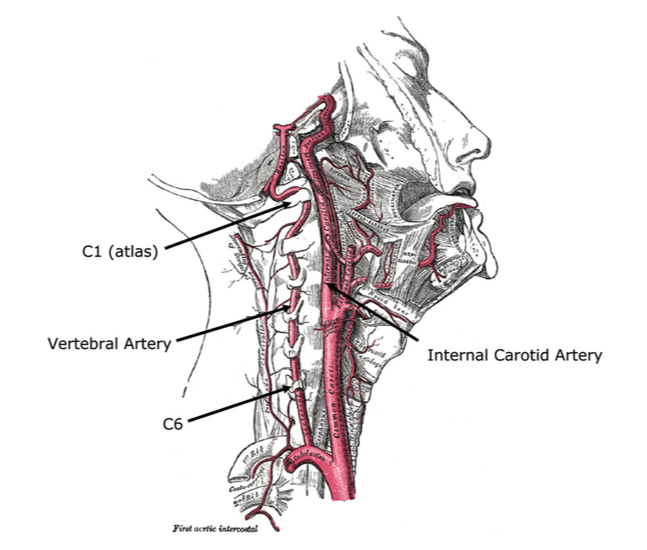
The vertebral artery arises from the subclavian artery and travels through the transverse foramina of C6 to C1, where it exists the vertebral foramina and pierces the atlanto-occipital membrane to enter into the foramen magnum. Due to the course of the vertebral artery it is vulnerable to compression during cervical rotation on the contralateral side. VBI is a familiar term to therapists describing the presents of posterior circulation ischemia due to vertebrobasilar insufficiency.
There are two ways in which the vertebral artery can be injured. The first is from pathology within the artery itself and the second from mechanical trauma. Although mechanical forces are applied to the artery during cervical movements and particularly cervical rotation/extension, little evidence exists to support that the manipulation is the cause of initial injury. Lesions in the vertebral artery become symptomatic if the contralateral vertebral artery does not accommodate for the occlusion of blood supply (Tinel et al., 2008, p. 406-407).
Dr. Percy discusses anomalies later in this blog but in short, there can be abnormal foramations in the circulation between the vertebral artery and basilar artery which lead to arterial incompetence. There can also we cardiovascular changes and pathology within the vertebral artery that results in stenosis, dissection or embolism leading to VAD. Cervical manipulation is not always to blame for such adverse effects but we often don't know who has underlying risk factors unless we specifically question for them. Predisposing factors may include hypertension, fibromuscular dyplasia, collagen vascular disease, or Marfans Syndrome. Research has started to suggest that more often the lesion in the vertebral artery is preexisting from past trauma or sporting injury to the cervical spine and the rotation movement in cervical manipulation exacerbates this rather than causing the initial lesion.
There are two mechanisms of injury associated with VAD; spontanteous injury and mechanical trauma (Taylor & Kerry, 2010). Spontaneous injury can be the result of cardiovascular disease or even viral meningitis, which results in inflammation in the arterial wall leading to weakness and a subsequent dissection (Dr. Percy). A less accepted but still possible mechanism is embolism from a pre-existing thrombosis on the arterial wall (Thiel & Rix, 2005, p. 155). Dr. Percy explains that there are two types of vertebral artery dissection.
- Steno-occlusive dissection occurs with dissection to subintimal plane with vessel luminal narrowing or occlusion.
- Dissecting aneuryms occur with dissection into subadventitial plane with dilatation of the outer wall. Focal or fusiform aneurysmal dilatation occurs with/ without stenosis.
The second mechanism of injury (and one I was more aware of) is cause by mechanical forces that alter the haemodynamics and affect circulation to the brain. This can be caused by direct trauma, such as a stab wound, or indirect trauma following a MVA, cervical spine or skull fracture, cervical manipulation, coughing and cervical hyperextension (seen with hair flicking). As there are many possible causes of vertebral artery injury, it is difficult to label the single predicting or responsible factor for VAD and more specifically, although there is a risk of injury with manipulation, manipulation should not take all the blame.
Course of the vertebral and internal carotid artery (Taylor & Kerry, 2010, p. 86)
One case study which I have found to be very helpful in understanding the 'worst case scenario' was published by Tinel and colleagues in 2008, and provides a detailed description a clinical case when VAD and stroke occurred in a patient complaining of neck pain. I would highly recommend reading this article to expand on your knowledge of the risks of cervical manipulation. There is a second article which I would recommend for developing a well rounded understanding of this topic, which discussed the different clinical presentation of vertebral artery dissection compared to carotid artery dissection (Taylor & Kerry., 2010 - see references).
Stoke is the most serious complication of cervical manipulation and often the most discussed, but there are other adverse events that can occur (Tinel, et al., 2008, p. 404).
- Neurovascular complications (Alternate Syndrome, Wallenberg Syndrome, Locked-in Syndrome).
- Neuro-orthopaedic complications (spinal cord injury, nerve root/trunk/plexus injury).
- Musculoskeletal complications (fracture, subluxation, cervical sprain and increased pain).
CLINICAL PRESENTATION OF VBI
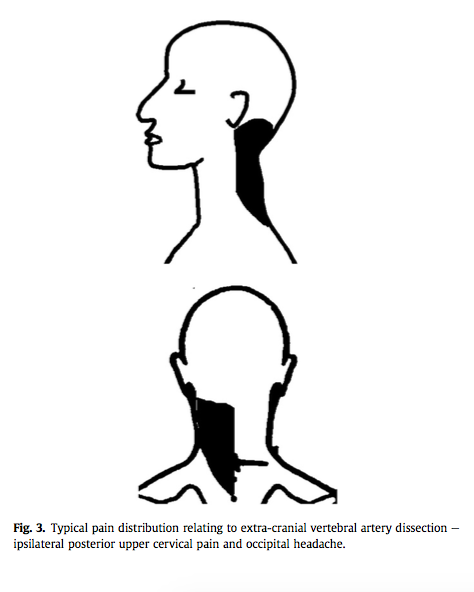
(Taylor & Kerry, 2010, p. 88)
There is a wide diversity in presentation of symptoms in people who present with VBI. VBI is caused by posterior circulation ischemia and patients can present with both ischemic and non-ischemic symptoms.
Hind-brain ischemic symptoms include dizziness, diplopia, dysarthria, drop attacks, dysphagia, nausea, nystagmus, fascial numbness, ataxia, loss of short-term memory, hoarseness, vagueness and limb hypotonia etc. (Taylor & Kerry, 2010).
Non-ischemic symptoms associated with VBI are similar to those presenting with a mechanical cervical spine disorder. 85% will present with headache, 67% with neck pain and 52% with dizziness (Gibbons & Tehan., 2015). These percentages are really high, which is why Physiotherapists need to be cautious and thorough in their assessment of patients with these symptoms. The following table provides a great summary of the clinical features of VAD and brainstem ischemia arising from compromised blood flow.
(Thien & Rix., 2005, p. 155)
identifying patients at risk of vBI
In 2006 the Australian Physiotherapy Associate (APA) released a revised clinical guidelines for assessing vertebrobasilar artery insufficiency in the management of cervical spine disorders. There is a three page appendix in this document that clearly outlines the questions to include in the subjective assessment.
The aim of the subjective assessment...
"Enquiry should also determine the nature of any neck pain or headache, which are usually the first symptoms of dissection of the vertebral artery. Specifically, sudden, severe, sharp pain located in the ipsilateral postero-superior region of the neck and occiput and for which there is no past history should be regarded as suspicious.
Patients may also report a history of cervical trauma or neck stiffness, and their neck range of motion can be restricted. Pain usually precedes ischaemic symptoms and signs, with the time interval varying among individuals. Until the ischaemic response becomes manifest it can be difficult to differentiate a dissecting vertebral artery from a benign mechanical neck disorder. It is therefore prudent to initially treat conservatively and carefully monitor progress.” (APA, 2006, p. 3)
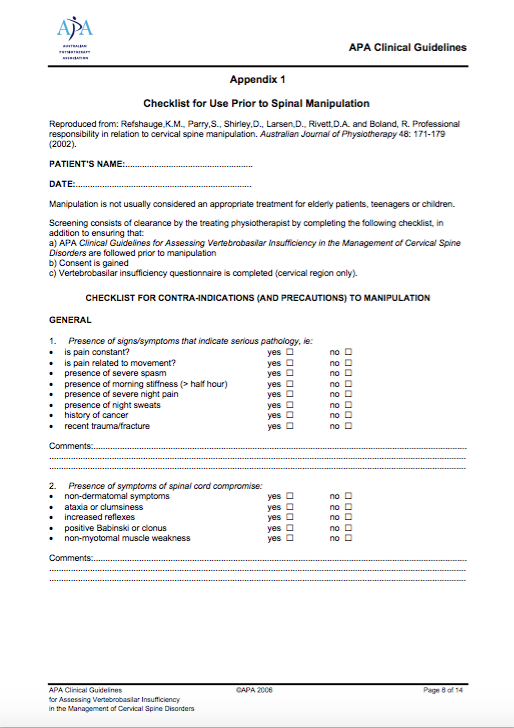
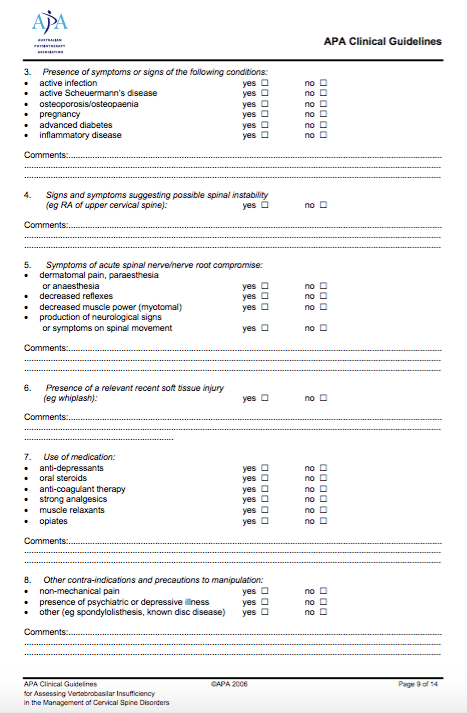

What you will notice from this appendix is that during the subjective assessment one must try:
- Establish the mechanism of injury and nature of the pain.
- Establish the location and aggravating/easing factors.
- Check for red flags 5D's and 3N's and other possible symptoms associated with VBI.
- Ask about other symptoms - tinnitus, arm symptoms, problems with gait etc.
- Ask about history of migraine and family history of migraine.
- Question about past history of neck trauma or injury.
- Thoroughly question about general health and medical history - particularly thrombolytic risk factors (see below), hypertension and other indicators of cardiovascular disease.
- Ask clearing questions to identify any conditions/symptoms that are contraindications to manipulation.
Dizziness has been shown to be highly associated with vertebral artery disease. In the study by Moubayed & Saliba (2009) 49% of the participants that reported isolated dizziness or vertigo had hypoplastic or stenotic vertebral arteries on medical examination, which is a really high percentage. Most of these patients also had at least three other stroke risk factors.
Thrombolic stroke risk factors include (Moubayed & Saliba, 2009, p. 2072):
- Age over 55
- Male sex
- Prior stroke or transient ischemic attack
- Ischemic heart disease
- Hypertension (treated or not)
- Diabetes (controlled or not)
- Lipid abnormalities (treated or not)
- Any cigarette smoking in past year
- Emotional stress
- Less than 4 hours of physical activity weekly
Validity of VBI tests
It was first postulated in 1927 that the combined effect of cervical rotation and extension would affect blood flow in the contralateral vertebral artery. Since that time, functional pre-manipulative screening has been used by manipulative therapists. However there remains a huge controversy about the validity of these pre-manipulative screening tests due to the large number for false negatives. Therapists perform these tests in an attempt to establish negligence protection, but it remains uncertain if the tests themselves can produce VBI (Thiel & Rix, 2005).
Diagnostic accuracy (Hutting, et al., 2013)
- Sensitivity from 0 to 57%
- Specificity from 67 to 100%
- Positive predictive value from 0% to 100%
- Negative predictive value from 26 to 96%.
- The positive likelihood ratio ranged from 0.22 to 83.25
- Negative likelihood ratio from 0.44 to 1.40.
In these studies the test being examined was combined rotation and extension, which was maintained for 10-30 seconds. The results were compaired against the reference tests of duplex and doppler ultrasound. As you can see from the wide range of values the diagnostic accuracy of the VBI tests variable and poor.
"In this sense, the provocative or functional vertebral artery insufficiency tests are considered to be a screen for otherwise unapparent vertebral artery pathology that may represent a pre-manipulation risk, in a situation where SMT of the cervical spine is considered to be the treatment of choice. By ‘unapparent’ we mean the absence of historical or other clinical features suggestive of vessel pathology such as dissection, and/or brainstem ischaemia. . .” (Thiel & Rix, 2005, p. 155)
From several studies evaluating arterial blood flow with Doppler studies it has become apparent that the postulated changes in blood flow thought to occur during the pre-manipulative screening do not always occur in the rotation/extension position, and therefore the validity of the these screening tests is questioned. Firstly, if the test does not fully evaluate the integrity of blood flow, then false negatives will occur, meaning that the safety of performing cervical manipulation has not been determined. Secondly, if there is a pre-existing defect in the vertebral artery and blood flow occlusion does occur, the tests themselves may be dangerous (Thiel & Rix., 2005).
"...the emphasis has shifted to greater weight being placed on interpretation of the findings elicited in the patient’s history, and substantially less on the results of the provocative tests themselves (Rivett et al., 2006). The provocative tests have not yet been discarded as the research evidence is not completely clear as to their value in detecting patients with vascular changes (Mitchell, 2007). There is still much debate in this regard (Thiel and Rix, 2005), and in the absence of a more valid alternative screening procedure it would seem somewhat premature to jettison them entirely.” (Rivett, 2008, p.e6)
In 2014 the American Heart Association published a scientific statement in the journal Stroke discussing risk of vertebral artery trauma and stroke risk associated with mechanical forces involved in cervical manipulation. Many patients who suffer from vertebral artery pathology will present with neck pain and headaches. They emphasise that while diagnostic imaging is helpful, there is no gold standard assessment in clinical assessment and all patients should be informed about the inherit risks associated with cervical manipulation. This scientific statement definitely placed cervical manipulation in a negative spotlight. The American Physical Therapy Association released a response to this scientific paper shortly after questioning the scope and context of this scientific paper in reducing stroke risk.
The APTA reinforce the message which is consistent with the APA and many research trials, that if the patient is comprehensively assessed and risk factors noted, that the risk of serious adverse events associated with cervical manipulation are minimised as much as possible. The tests themselves for VBI lack clinical validity and are in no way a gold standard assessment, but, they the only tests currently available to assist with patient assessment. Just because the research remains inconclusive doesn't mean that cervical manipulation is completely unsafe and should be avoided. It is definitely a case of picking the most appropriate patient and deciding what the best treatment choices are for them. It relies on the Physiotherapist having a broad knowledge of questioning, differential diagnosis and solid clinical reasoning skills.
"The risk of a post manipulation serious accident is regarded as reduced if the contraindications for the manipulation are respected and the technology in agreement with best practice” (Tinel, et al., 2008, p.404).
The role of medical imaging
After reading the current research debating wether pre-manipulative screening is safe, valid and effective, I wanted to learn more about the role of medical imaging discussed in these articles. The consequences are VBI are too high to risk missing the opportunity for adequate medical treatment for vertebral artery disease. I asked Dr. Percy what his opinion was around this topic.
Dr. Percy's explains the role of XRAY and Doppler US examination.
"X-Rays are the mainstay of Radiology and are frequently the initial imaging assessment of a patient with neck pain, headaches, or symptoms such as dizziness. If you wish or need to image the vertebral arteries and the posterior circulation ( vertebral and basilar arteries ), anterior circulation (common and internal carotid arteries) and the intracranial vessels; then one can start with a Doppler ultrasound exam. This will look at the common and internal carotid arteries, assess the amount of intimal thickening that may be present, look for soft and hard atheromatous plaque, and assess the degree of arterial narrowing that is present, if at all. Soft plaque is a concern as may rupture and become a source of emboli.
The Doppler US can see the direction and velocity of flow in the vertebral arteries, but they are more difficult to see as they run up the neck through the transverse foramina. It is good to document that there is prograde flow i.e. towards the brain, and not retrograde flow which would indicate the presence of a steal phenomenon. Vertebral steal phenomenon occurs when there is a high grade stenosis or occlusion of the subclavian artery (usually left) proximal to the origin of the vertebral artery, and thus the vertebral supplies blood flow to the subclavian vessel via the circle of Willis in the brain if it is competent.
The best imaging technique for evaluating the vertebral arteries is CT angiography and MR angiography using frequency contrast, not non-contrast. One wants to make sure that the arteries are both patent (one is usually dominant and larger than the other), that there is no occlusion or stenosis, nor mass effect for degenerative changes of the cervical vertebrae and facets etc.
The non-dominant vertebral artery frequently in my experience, terminates in the Posterior Inferior Cerebellar Artery ( PICA ) while the dominant vessel supplies the basilar and possibly the Posterior Cerebral Arteries if they arise from the basilar artery. The posterior cerebral arteries often have a 'primitive origin' and arise from the terminal internal carotid arteries. They usually but not always, communicate with the basilar artery if they arise from the ICA. One may arise from the ICA, the other from the Basilar artery. If the posterior cerebral artery, which has arisen from the ICA, does not communicate with the basilar, OR if the posterior cerebral artery arising from the basilar does not communicate with the ICA via the posterior communicating artery then the circle of Willis is not competent. This can create serious problems if there is an arterial occlusion or dissection i.e. the circle of Willis cannot compensate and supply the intracranial end vessels. Medical imaging is therefore vital to determine the risk of cervical manipulation causing arterial trauma and vertebral artery dissection."
Moubayed and Saliba conducted a high quality trial to explore the pathology of vertebral artery and the correlation of pathology to dizziness/vertigo and VBI. Despite the quality of this trial the authors concluded that the sensitivity of physical examination is low (47%) (2009, p. 2075), and recommended that imaging should be performed in all patients “suffering from isolated positional vertigo or dizziness of unexplained aetiology and having at least three stroke risk factors.
The current gold standards for imaging include contrast-induced MRA and CTA. 'The sensitivity of MRA, CTA, and Doppler ultrasound is 93.9%, 100%, and 70.2%, respectively. The specificity for MRA, CTA, and Doppler ultrasound is 94.8%, 95.2%, and 97.7%, respectively' (Moubayed & Saliba, 2009, p. 2075). These statistics support and strengthen the recommendations from Dr. Percy.
Conclusion
Hopefully this blog has highlighted the controversy and debate that continues around the topic of VBI. You may be wondering what to do with this information and what the best actions to take are?Taylor & Kerry (2010, p. 91-92) provide a fantastic list of recommendations to guide the actions of Physiotherapists:
- Expand manual therapy theory to encompass a ‘systems based’ approach, incorporating the whole cervical vascular system, including the carotid arteries.
- Expand manual therapy theory and practice to include haemodynamic principals and their relationship to movement anatomy and biomechanics i.e. what happens to the vertebral artery during movement.
- Enhance subjective/objective examination:
- Include questioning about cardiovascular disease such as hypertension and know how questioning reflects function of the cranial nerves (5D's and 3N's)
- Develop a high index of suspicion for cervical vascular pathology, particularly in cases of acute trauma.
- Develop increased awareness that neck pain and headache may be precursors to potential posterior circulation ischemia.
- In cases of acute onset headache “unlike any other” couples with ambiguous examination findings, retain an index of suspicion and use conservative or gentle treatment techniques in the early stages of management.
- Develop an awareness of the limitations of current objective tests such as pre-treatment movement testing.
- Where frank arterial injury is suspected prior to or following a treatment intervention, immediate triage to an appropriate emergency centre is recommended, together with a report on any treatment methods undertaken.
I'd like to thank Dr. Percy for taking the time to share his recommendations with me for this blog. It is so important for Physiotherapist's to know that there are proven inherent risks associated with cervical manipulation. It is also reassuring to know how medical imaging can assist with our clinical assessment of a patient presenting with neck pain, dizziness and headache. No matter how small the risks are, there is still no certainty that our assessment can mitigate all risk.
Sian
References
Biller, J., Sacco, R. L., Albuquerque, F. C., Demaerschalk, B. M., Fayad, P., Long, P. H., ... & Tirschwell, D. L. (2014). Cervical Arterial Dissections and Association With Cervical Manipulative Therapy A Statement for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke, 45(10), 3155-3174.
Carlesso, L., & Rivett, D. (2011). Manipulative practice in the cervical spine: a survey of IFOMPT member countries. Journal of Manual & Manipulative Therapy, 19(2), 66-70.
Gibbons, P. & Tehan, P. 2015, In Touch, p. 16-18.
Hutting, N., Verhagen, A. P., Vijverman, V., Keesenberg, M. D., Dixon, G., & Scholten-Peeters, G. G. (2013). Diagnostic accuracy of premanipulative vertebrobasilar insufficiency tests: a systematic review. Manual therapy, 18(3), 177-182.
Kerry, R., & Taylor, A. J. (2006). Cervical arterial dysfunction assessment and manual therapy. Manual therapy, 11(4), 243-253.
Kerry, R., Taylor, A. J., Mitchell, J., & McCarthy, C. (2008). Cervical arterial dysfunction and manual therapy: a critical literature review to inform professional practice. Manual Therapy, 13(4), 278-288.
Kerry, R., Taylor, A. J., Mitchell, J., McCarthy, C., & Brew, J. (2008). Manual therapy and cervical arterial dysfunction, directions for the future: a clinical perspective. Journal of Manual & Manipulative Therapy, 16(1), 39-48.
Maitland, G. D. (2005). Maitland's vertebral manipulation (Vol. 1). E. Hengeveld, K. Banks, & K. English (Eds.). Butterworth-Heinemann.
Moubayed, S. P., & Saliba, I. (2009). Vertebrobasilar insufficiency presenting as isolated positional vertigo or dizziness: A double‐blind retrospective cohort study. The Laryngoscope, 119(10), 2071-2076.
Rivett, D. (2008). Letter to the editor response. Manual Therapy, 13(3), e6.
Rushton, A., Rivett, D., Carlesso, L., Flynn, T., Hing, W., & Kerry, R. (2014). International framework for examination of the cervical region for potential of cervical arterial dysfunction prior to orthopaedic manual therapy intervention.Manual therapy, 19(3), 222-228.
Taylor, A. J., & Kerry, R. (2010). A ‘system based’approach to risk assessment of the cervical spine prior to manual therapy. International Journal of Osteopathic Medicine, 13(3), 85-93.
Thiel, H., & Rix, G. (2005). Is it time to stop functional pre-manipulation testing of the cervical spine?. Manual Therapy, 10(2), 154-158.
Tinel, D., Bliznakova, E., Juhel, C., Gallien, P., & Brissot, R. (2008, June). Vertebrobasilar ischemia after cervical spine manipulation: a case report. InAnnales de réadaptation et de médecine physique (Vol. 51, No. 5, pp. 403-414). Elsevier Masson.