Thoracic Outlet Syndrome
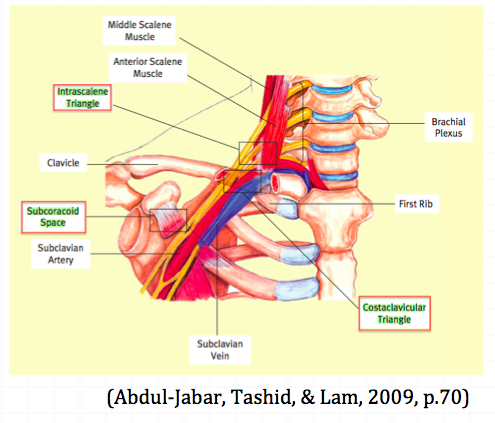
Thoracic outlet syndrome (TOS) is a syndrome/condition that encompasses cluster of upper extremity symptoms which are due to compression of the neurovascular bundle by various structures in the area just above the first rib and behind the clavicle. The three most common regions where compressions is thought to occur is the intrascalene triangle, the costoclavicular triangle and the subcoracoid space.
The term thoracic outlet syndrome describes a cluster of symptoms sitting on a continuum ranging from intermitted postural symptoms to severe/permanent neurological/vascular deficits. (Hooper, Denton, McGalliard, et al., 2010a; Sanders, Hammond, & Rao, 2007; Watson, Pizzari, & Balster, 2009, Kaczynski, & Fligelstone, 2013)
Thoracic outlet syndrome was first described in 1927 by Adson and colleagues and known at this time as scalenus anticus syndrome. The formal term that most authors refers to as Thoracic outlet syndrome was derived by Peet and colleagues in 1956. When reviewing literature in the topic of TOS keep an open mind that the condition itself and subject population are often poorly defined and vary enormously between studies. This leads to poor study results due to the heterogeneity of the study population.
If you are reading about TOS you might noticed that there is always an element of controversy about it's definition, diagnosis and treatment. Let's take a look at these points of controversy in closer detail. The first point of controversy is that the definition does not specify where or what or how compression occurs. The second point of controversy revolves around the diagnosis of symptomatic TOS, where no radiological or electrophysical abnormalities can be detected and the pathological cause for symptoms is unknown. Diagnosis will rely heavily on physical examination and collection of objective asterisk signs for reproduction of symptoms. And, the third point of controversy is about the lack of a clear definition of the clinical presentation of TOS. Many patients may present with a cluster of arterial, venous, neurogenic and pain symptoms and diagnosis relies on clinical reasoning of the assessing therapist. Below are some of the key features of TOS that I found consistently throughout the literature to be present in this condition.
Classification of Thoracic outlet syndrome
In the current research trials, thoracic outlet syndrome is being classified into the following categories:
- The first category is Vascular TOS, which includes arterial and venous and accounts for ~ 5% of all presentations.
- The second category is Neurological TOS, which is broken down further into true and symptomatic TOS.
- Symptomatic TOS comprises over 80% of all people presenting with this diagnosis. That is to say there is a huge proportion of patients will present with no radiological or electrophysical abnormality (Hooper et al., 2010a; Sanders et al., 2007; Kaczynski et al., 2013).
Aetiology
There are a number of reasons that TOS can occur. Most of the time, regardless of the mechanism, symptoms are caused due to an alteration in the shape of the thoracic outlet. This is referred to in more recent studies as container dysfunction (Hooper, et al., 2010a).
In the study by Kaczynski and colleagues (2013), which assessed the cause of compression in patients with vascular and true neurological TOS, over 80% were found to have fibrous muscular bands and hypertrophic scalene muscle. Cervical ribs and a broadened first rib only found in 3% of patients. However, in patients with symptomatic TOS these structural anomalies are often not found. It is speculated therefore, that the mechanism of symptoms relates to altered breathing mechanics, postural dysfunction, scapular dyskinesia, muscular imbalances and neural tension.
The prevalence is thought to be 8% in the general population and present between the ages of 18-60+ years old. Women are 3-4 times more likely to suffer from TOS symptoms and this conditions is rarely seen in children. It is reported in up to 50% of cases of Carpal Tunnel syndrome, as double crush syndrome (Hooper, et al., 2010a; Watson, et al., 2009).
Diagnosis & Clinical presentation
The diagnosis of thoracic outlet syndrome remains disputed as there is no standard objective test to confirm clinical impressions. It remains a diagnosis of exclusion (Hooper, et al., 2010, p. 76).
“Diagnosis of symptomatic thoracic outlet syndrome is dependent on a systematic, comprehensive upper-body examination” (Watson et al, 2009, p.588).
Watson and colleagues provide a two-part masterclass which comprehensively outlines the musculoskeletal examination required to arrive at the diagnosis of TOS, and provide treatment strategies to manage scapular dyskinesia, muscular imbalances and improve container dysfunction. It was one of the best sources I came across in this body of research and applicable to every day clinical practice. For further reading on clinical presentation, diagnosis and management I would refer you to these two articles.
Watson, L. A., Pizzari, T., & Balster, S. (2009). Thoracic outlet syndrome part 1: Clinical manifestations, differentiation and treatment pathways. Manual therapy, 14(6), 586-595.
- Watson, L. A., Pizzari, T., & Balster, S. (2010). Thoracic outlet syndrome Part 2: Conservative management of thoracic outlet. Manual therapy, 15(4), 305-314.
Distribution of symptoms
Symptoms can involve the head, neck, thorax and upper limb. Be sure to map the distribution of symptoms carefully on a body chart as this may help with differential diagnosis (Hooper et al, 2010a). To further understand the difference between arterial, venous, neurogenic and pain symptoms I would recommend Hopper et al (2010a), who provide a clear table outlining the individual symptoms and cross over between categories.
- Arterial symptoms: pain (mostly in the hand), numbness which is non-radicular, coolness to touch, cold intolerance and pale discolouration. Mostly seen in a younger population involved in repetative overhead activity.
- Venous symptoms: excruciating chest pain, cyanotic discolouration, distended collateral veins and oedema in the extremity.
- Neurogenic Symptoms: pain, paraesthesia, numbness and weakness involving the neck, shoulder and upper limb. Symptoms are often preceded by neck trauma, MVA or repetative stress through work/sport. True neurological weakness will be present in true TOS, while many have symptoms of clumsiness and loss of dexterity.
- Pain
- Paraesthesia is most commonly reported in the 4th and 5th fingers if the lower trunk of the brachial plexus is involved. Depending when the compression of the brachial plexus occurs will cause variation in symptoms.
Establish severity, irritability, nature, and 24 hour behaviour.
Aggravating positions
- Sustained shoulder elevation or sustained activities.
- Repetitive use of the upper limb.
- Lying on the arm.
- Carrying a bag or backpack.
- Prolonged postures.
Physical examination is long and requires a comprehensive assessment of the cervical and thoracic spine and upper quadrant, including:
- Active and passive range of movement looking for reproduction of symptoms.
- Breathing technique
- Resting posture and observation of skin discolouration or swelling.
- Assessment of scapular motor control.
- Upper limb neurodynamic assessment
- Upper limb neurological examination.
- Palpation, in particular the cervical spine and supraclavicular fossa.
- Shoulder special testing for rotator cuff pathology and glenohumeral joint instability.
- Peripheral nerve testing (for carpal tunnel syndrome and other peripheral entrapment neuropathies).
- Muscle length and strength of the cervicobrachial muscles.
Pain Provocation tests
As mentioned above there is no standard clinical test that confirms the diagnosis of TOS. There are however five available pain provocation tests which can be used as a group of tests to provide symptoms. None of these tests are valid as a single entity but studies have been conducted that show 3-4 positive tests have a sensitivity of 85-90% and specificity of ~30%. To increase the specificity to 84% you need all five positive tests (Gillard, Perez-Cousin, Hachulla, et al., 2001, p.419). For further detail on these tests refer to Abdul-Jadar, 2009 and Watson, et al., 2009.
- Wright's test
- Known also as the hyper-abduction manoeuvre.
- The arm is held in 90 degrees abduction and external rotation, 45 degrees elbow flexion and sustained for 1 minute.
- Adson's test
- The patient holds their arm to the side and turns the head to full rotation and extension to the ipsilateral side. The patient is asked to breathe in deeply.
- Costoclavicular test
- The patient is positioned in scapula retraction, depression, elevation and protraction and held in each position for up to 30 seconds.
- Roos Test
- Performed by holding both arms in an elevated and abducted position with elbows bent to 90 degrees.
- The patient is then instructed to open and close their hands repeatedly for 3 minutes.
One thing to keep in mind is that the above tests is that when the clinical validity was examined it was done so on healthy individuals. Meaning that, many people will have a positive test without symptoms and there is no normative data available for these tests. A second point to keep in mind is that the tests are considered positive if there is an obliteration of the radial pulse. To sustain the test until the pulse is lost may be unnecessary and too aggressive. Many authors now suggest performing them until reproduction of symptoms.
Clinical Prediction Rule
Lindren et al (1997) produced a clinical prediction rule stating that the clinical diagnosis can be made with at least ¾ of the following symptoms;
- Aggravation with arm in elevated position.
- Paraesthesia originating from C8/T1.
- Supraclavicular tenderness over brachial plexus.
- Positive Roos test.
With current research we know that a more thorough examination is required and Gillard et al (2001) suggest 3-4 positive pain provocation tests in this rule. This clinical prediction rule can still be implemented as a rough guideline by clinicians to aid in the clinical reasoning process.
Following the extensive physical examination there should be enough objective measures taken to allow for differential diagnosis of the following conditions. Often patients will be referred for further diagnostic measures such as MRI, nerve conduction studies, doppler ultrasound, angiography, venous ultrasound, Helical CT angiography and even plain XRAY to further investigate the degree of neurovascular compromise and identify any contributing patho-anatomy. It is important to remember than no single test can be used as a standard reference.
Differential diagnosis (Watson et al., 2009, p.589):
- Carpal tunnel syndrome or other peripheral neuropathies.
- De Quervain's tenosynovitis.
- Lateral epicondylalgia & Medial epicondylalgia.
- Complex region pain syndrome.
- Horner's syndrome.
- Raynaurd's disease.
- Cervical spine disc pathology, spondylolisthesis or spondylosis causing cervical radiculopathy
- Brachial plexus trauma.
- Systemic inflammatory disease or cardiac disease.
- Upper extremity deep vein thrombosis.
- Pagets-Schroetter syndrome.
- Rotator cuff pathology.
- Glenohumeral joint instability.
The second part of this blog will cover information regarding the current trends in physiotherapy management for Thoracic outlet syndrome including scapular retraining and clinical neurodynamics.
Sian
References:
Abdul-Jabar, H., Rashid, A., & Lam, F. (2009). Thoracic outlet syndrome. Orthopaedics and Trauma, 23(1), 69-73.
Gillard, J., Perez-Cousin, M., Hachulla, E., Remy, J., Hurtevent, J. F., Vinckier, L., et al. (2001). Diagnosing thoracic outlet syndrome: contribution of provocative tests, ultrasonography, electrophysiology, and helical computed tomography in 48 patients. Joint bone spine, 68(5), 416-424.
Hooper, T. L., Denton, J., McGalliard, M. K., Brismée, J.-M., & Sizer Jr, P. S. (2010). Thoracic outlet syndrome: a controversial clinical condition. Part 1: anatomy, and clinical examination/diagnosis. The Journal of manual & manipulative therapy, 18(2), 74.
Hooper, T. L., Denton, J., McGalliard, M. K., Brismee, J. M., & Sizer, P. S., Jr. (2010). Thoracic outlet syndrome: a controversial clinical condition. Part 2: non-surgical and surgical management. The Journal of manual & manipulative therapy, 18(3), 132-138.
Kaczynski, J., & Fligelstone, L. (2013). Surgical and Functional Outcomes After Thoracic Outlet Syndrome Decompression via Supraclavicular Approach: A 10-Year Single Centre Experience. Journal of Current Surgery, 3(1), 7-12.
Lindgren, K.-A. (1997). Conservative treatment of thoracic outlet syndrome: a 2-year follow-up. Archives of physical medicine and rehabilitation, 78(4), 373-378.
Mackinnon, S. E., & Novak, C. B. (2002). Thoracic outlet syndrome. Current Problems in Surgery, 39(11), 1070-1145.
Peet, R. M., Henriksen, J. D., Anderson, T., & Martin, G. M. (1956). Thoracic-outlet syndrome: evaluation of a therapeutic exercise program. Paper presented at the Proceedings of the staff meetings. Mayo Clinic.
Roos, D. B. (1990). The thoracic outlet syndrome is underrated. Archives of neurology, 47(3), 327.
Sanders, R. J. (2013). Anatomy of the Thoracic Outlet and Related Structures Thoracic Outlet Syndrome (pp. 17-24): Springer.
Sanders, R. J., Hammond, S. L., & Rao, N. M. (2007). Diagnosis of thoracic outlet syndrome. Journal of vascular surgery, 46(3), 601-604.
Watson, L. A., Pizzari, T., & Balster, S. (2009). Thoracic outlet syndrome part 1: Clinical manifestations, differentiation and treatment pathways. Manual therapy, 14(6), 586-595.
Watson, L. A., Pizzari, T., & Balster, S. (2010). Thoracic outlet syndrome Part 2: Conservative management of thoracic outlet. Manual therapy, 15(4), 305-314.