Cervical Radiculopathy Part 3 - Physiotherapy Treatment
We've made it to part 3 - treatment for cervical radiculopathy. If you missed them, please check out the blogs on subjective examination and physical examination. I'm going to begin this blog by saying that when it comes to treatment, there is no clear guideline for the optimal conservative management for radiculopathy. I read many papers and systematic reviews and have extracted ideas for treatment strategies to share with you. Before you begin deciding which treatment to use, you first need to decide on the goals for treatment:
- Pain relief
- Reduced muscle tension
- Improved range of movement
- Improved functional levels
- Restoration of neurological function
- Prevention of reoccurrence
- These are all possible goals and will depend on the outcome of both your subjective and objective examination.
- Another way to think about it is to ask if you need to improve the health of the nerve or restore healthy mechanics for the nerve to move well again?
After deciding what your goals are, you need to consider what avenue of treatment is best for your client. There are three main routes for treatment:
- Conservative
- Pharmacological
- Surgical
“The majority of patients diagnosed with cervical radiculopathy (75-80%) will improve with non-operative management” (Caridi, Pumberger & Hughes., 2011, p. 268).
I love this statement because it is so optimistic and positive. But then I thought what do they mean by conservative treatment? So I began reading and soon realised that a concrete answer to that question does not exist. The way in which I manage cervical radiculopathies was taught to me by senior Physiotherapists and mentors from my previous job. I generally have good results with treatment outcomes and so never have thought to question where they got those ideas from. Now I see, it is often a compilation of treatments, a combined approach, and a utilisation of different treatments at different stages of recovery that results in the best outcomes. This blog will discuss the different therapies that are considered 'conservative' as well as pharmaceutical and surgical management for this condition.
conservative treatment
Overall I would say that I was slightly disappointed from reading many of the systematic reviews and papers comparing treatment options for cervical radiculopathy. When you read the abstract you are often lead to believe that for example, there is limited evidence to strongly recommend a set Physiotherapy treatment for this condition. However, when I went through and read many of the reviews or original papers, there is often no detail about what ‘Physiotherapy’ is, what ‘manual therapy’ or ‘general exercise’ constitutes. I’m sure you’ll agree that we all have different approaches for managing problems, and I was hoping for a bit more guidance from the current literature, but I found a small handful of papers that provided enough detail that I could actually reproduce clinically what they had evaluated.
Another point to notes is that many of the systematic reviews which are conducted over a 10+ year time period often only find <5 articles that satisfy the inclusion criteria. This suggests that we are still lacking in high quality and consistently reproducible papers about treatment approaches. If each researcher explores a different therapy then it is difficult to evaluate and compare approaches and then implement them in clinical practice.
There are both passive and active treatments we can use. Passive mostly consists of the cervical soft collar, patient education and rest. Active treatment consists of manual therapy, exercise and mechanical traction.
Soft collar
I’ve used them clinically when patients find relief with manual traction and they are unable to find a position of relief independently. The aim is to reduce pressure on the nerve root and improve the pathophysiology resulting from compression i.e. the health of the nerve. Essentially once the collar has been fitted I would expect my patient to tell me there is an immediate reduction in there symptoms, not complete resolution but a definite change. They also have to be compliant in wearing it so they can get relief from the pain and let their neck rest. It should be noted however, that prolonged collar use beyond 2 weeks has been shown to result in muscle deconditioning (Caridi, Pumberger & Hughes., 2011, p. 268).
patient education
Education is obviously specific to the person you are treating but there are a few things I try to remember to discuss with them.
- I generally recommend minimal driving because it can be difficult to check their blind spot and you don’t want them to have an accident or continue aggravating their neck from turning too far into painful range.
- I try to educate them about typical aggravating and easing factors as well as appropriate positions for rest and sleeping.
- I encourage them to follow the guidelines given by their doctor/pharmacist for each medication and not to stray from the dosage.
Cervical traction
Traction is an interesting one because many clinics don't actually have a mechanical traction unit. Where I worked previously we did and I used it quite a lot, with great outcomes. “Some studies have shown mechanical traction to be effective within the first 6 weeks of injury” (Caridi, Pumberger & Hughes., 2011, p. 268). “Five studies have looked at traction as a treatment for radiculopathy. All five showed that traction was temporarily efficacious in relieving patient’s symptoms; however, none of the studies included standardized outcome measures” (Caridi, Pumberger & Hughes., 2011, p. 268).
Raney et al (2009) looked to identify which patients with neck pain (not just cervical radiculopathy) would benefit from cervical traction and exercise. Patients in this study had the following symptoms:
- Peripheralisation of symptoms with lower cervical mobility testing between C4-7.
- +ve shoulder abduction test
- >55 years of age
- +ve ULTT1
- +ve neck distraction test
As you can see these are all symptoms common in cervical radiculopathy. If 4/5 of these variables were present there was a ~95% chance of improvement following cervical traction. These patients received mechanical traction. No papers I read evaluated the over-the-door traction unit or manual traction and perhaps this is because it is hard to objective about the force you are placing through the neck? I suppose you can use manual traction but if you have a unit available, I would recommend mechanical traction.
Cervical traction is usually performed:
- Intermittent ration i.e on/off for 60 seconds on/20 seconds off.
- 2 x week for 3 weeks i.e 6 sessions.
- 15 minutes treatment duration.
- Average weight can range between 12-38 pounds but a good starting point is 10-12 pounds (5kg) and never go > 40 pounds.
- Cervical flexion of 24 degrees or 15 degrees if flexion is impaired.
- Supine lying with legs supported on box.
- Some authors say to begin with 9kg or 10% BW, which ever is less but I have always begun around the 5kg region.
Patients in this study also completed seated and supine DCNF exercises consisting of 10 second holds, twice and hour in sitting and 10 times a day when in supine (Raney, et al., 2009). We will discuss exercise prescriptions further on.
manual therapy
From what I have read, the term 'manual therapy' for cervical radiculopathy often refers to cervical or thoracic manipulation. The use of cervical manipulation is lacking in high quality evidence for its long term benefit (Corey & Comeau., 2014; Caridi, et al., 2011). This is not my clinical preference as patients are often too irritatable and lack the appropriate range of movement to get into position.
In 2011, Leininger, Bronfort, Evans and Reiter published a systematic review evaluation the efficacy of mobilization and manipulation for radiculopathy. Their conclusions stated “Evidence for STM and/or MOB for the cervical spine-related extremity symptoms is very low in quality for all included comparison treatments. Thus, conclusions regarding effectiveness cannot be made” (Leininger, et al., 2011, p. 110).
My reluctance with manipulation is that all patients require a full assessment to determine the safety and risk of performing this treatment. Normally, when a patient presents with cervical radiculopathy they do no have the range of cervical rotation to comfortably get into the pre-manip position. So if I can’t have confidence that they will tolerate the treatment technique, I am not going to use it. It is too hard to rule out the contraindications for movement. “Given the risks involved with manipulation and the paucity of evidence showing any benefit, this therapy cannot be recommended as a predictable treatment option” (Caridi, Pumberger & Hughes., 2011, p. 268).
Exercise therapy
“While there is little evidence to suggest which non-operative treatment approach is best for the management of patients with cervical radiculopathy, emerging evidence suggests that these patients benefit from a multimodal treatment approach.” (Costello, 2008, p. 129)
There are a few papers discussing manual therapy and exercise therapy that I can share with you. Costello (2008) wrote a case study describing how a combined treatment of thoracic spine thrust manipulation, soft tissue treatment, and therapeutic exercise over three sessions resulted in significant reduction in pain rating scores and patient perceived function and disability. Looking deeper into the definition of ‘therapeutic exercise’ it appears that Costello implement:
- DCNF in supine 10 second holds x 10 repetitions.
- Prone Scapula retraction 10 sec holds x 10 repetitions.
- Pec stretches in the doorway at a comfortable level x 10 repetitions.
- Median nerve slider 5-10 repetitions in a painfree range.
- All exercises were performed 3 times a day. Costello describes the progression of these day 1 treatments in his case study.
I really enjoyed reading this paper and how it was laid out to cover assessment, diagnosis, and progression of treatments over the three sessions with rational and discussion of his approach.
Cleland, Whitman, Fritz & Palmer (2005) presented a different treatment approach to that of Costello (2008) which included the following treatments:
- Cervical lateral glide with the limb placed in a neurodynamic position consisted with ULTT1 (median nerve bias).
- DCNF in supine without BFU for 10 second holds x 10 repetitions.
- Lower trapezius strengthening in prone with the arms in 120 degrees horizontal abduction.
- Middle trapezius strengthening in prone with the arms at 90 degrees abduction.
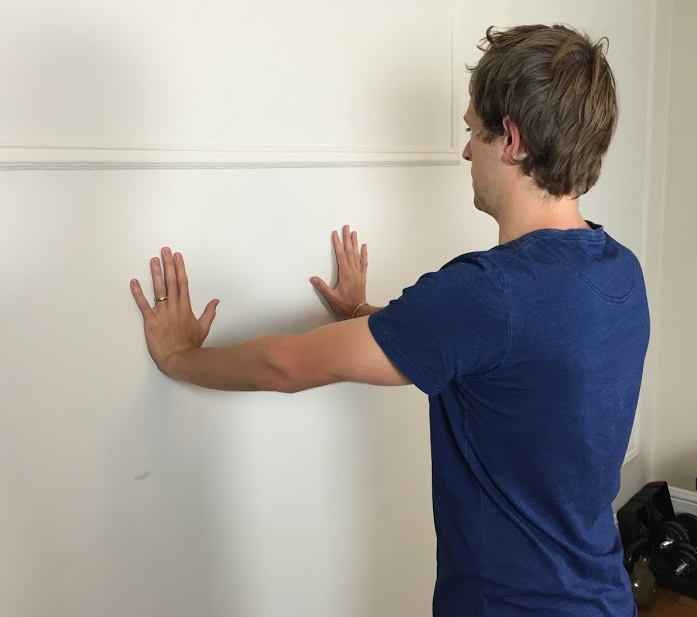
- Serratus anterior strengthening with wall push ups focusing on push up plus movement.
- Cervical mechanical traction for 15 minutes, 8.2 kg on 30 seconds : 5.4kg off 10 seconds, in 25 degrees cervical flexion.
- Thoracic spine thrust manipulation.
What I would like to draw attention to are the words ‘postural education’ and ‘manual therapy’ which are all terms used in the papers. For this topic, manual therapy often refers to thoracic manipulation or cervical glides in a neurodynamic position. Exercise can include anything from cervical retraction, cervical extension, DCNF strengthening, scapula retraction, lower and middle trapezius strengthening or serratus anterior strengthening. The main thing I wish for you to remember is that it is sometimes hard to find the details about what treatments were used and I would like to encourage you to go back to original papers and sift through for the finer details before taking the outcome of the abstract verbatim. Without the detail we don’t know how to change our clinical practice to align it with what the evidence says.
Pharmacotherapy
Pharmacotherapy usually includes a 1-2 week trial of NSAIDS. From there other medication prescribed include oral steroids, Lyrica and Effexor. There is insufficient evidence to support the use of these medications beyond a 2 month period (Corey & Comeau., 2014, p. 796)
From experience, I have seen significant improvements in pain and function when patients with a diagnosis of cervical radiculopathy are the prescribed one or a combination of these three medications. If they don’t have a good short term effect then I have not seen them provide long term relief, which correlates with the information above.
Cervical corticosteroid injection under radiographic guidance is another treatment option. They also fall under the realm of non-operative therapies but again there is no clear criteria for referral. Translaminar or transforaminal approaches can be used. “Retrospective and prospective studies show up to 60% of patients experience relief of radicular symptoms following corticosteroid injection” (Corey & Comeau., 2014, p. 796). This means they have been shown to have a good short-term reduction in pain but it is difficult to evaluate the long-term effects of these injections.
Surgical treatment
“There is a lack of high quality evidence comparing non-operative and surgical intervention in the treatment of cervical radiculopathy” (Corey & Comeau., 2014, p. 797). “General practice deems that patient’s with clinically significant motor deficits, debilitation pain that is resistant to conservative modalities and/or time, or instability in the setting of disabling radiculopathy are indicated for surgery” (Caridi, Pumberger & Hughes., 2011, p. 268).
“Urgent surgery is required in the presence of traumatic instability or injury but there is no strict criteria for following this course of action” (Caridi, Pumberger & Hughes., 2011, p. 268). I’d suspect however that those with traumatic injury and instability are more likely to present to ED that in a primary care setting. The surgery that many of these papers are referring to is anterior cervical decompression and fusion (Engquist, et al., 2013).
“Surgery for cervical radiculopathy followed by physiotherapy resulted in a more rapid improvement in neck pain than physiotherapy alone, but after 24 months there were few differences between groups. Thus a comprehensive physiotherapy program should be tried before surgery for patients with cervical radiculopathy” (Grotle & hagen., 2014, p. 24). This is an example of a concluding statement from a research paper comparing physiotherapy to combined surgery and physiotherapy. What you don’t interpret from this statement is that the subjects all received anterior decompression and fusion on the basis that disc herniation was the cause of the cervical radiculopathy. As mentioned in the first blog, we suspect for this condition that cervical spondylosis is the major cause of cervical radiculopathy and therefore these results need to interpreted in the context from which they came.
conclusion
In summary, cervical radiculopathy is a condition characterised by shoulder and arm radicular pain, altered neurological function, altered neurodynamic movement and dysfunction in cervical spine range of movement. Nerve root compression of the lower cervical spine is most common and pain is caused by compression of the dorsal root ganglion. To diagnose this condition clinically, you need to have a thorough understanding of the pain distribution and behaviour of symptoms. While there are many tests you can perform in the physical examination, a clinical prediction rule does exist to help guide us. Medical imaging and surgery are not first line treatments and conservative treatment including mechanical traction, manual therapy and exercise are considered to be effective treatments for this condition. I hope these past three blogs have helped to demystify this condition which can be a bit daunting as patients present with severe pain and limited function. I really enjoy treating spinal conditions and radiculopathies as every patient is so different and unique. Stick to the foundations of assessment and reasoning, and you'll find that the treatment becomes more clear.
Good luck, Sian :)
References
Anonymous. Pain in the neck and arm: a multicentre trial of the effects of physiotherapy, arranged by the British Association of Physical Medicine. Br Med J. Jan 29 1966;1(5482):253–258.
Carette, S., & Fehlings, M. G. (2005). Cervical radiculopathy. New England Journal of Medicine, 353(4), 392-399.
Caridi, J. M., Pumberger, M., & Hughes, A. P. (2011). Cervical radiculopathy: a review. HSS journal, 7(3), 265-272.
Cheng, C. H., Tsai, L. C., Chung, H. C., Hsu, W. L., Wang, S. F., Wang, J. L., ... & Chien, A. (2015). Exercise training for non-operative and post-operative patient with cervical radiculopathy: a literature review. Journal of physical therapy science, 27(9), 3011.
Cleland, J. A., Fritz, J. M., Whitman, J. M., & Palmer, J. A. (2006). The reliability and construct validity of the Neck Disability Index and patient specific functional scale in patients with cervical radiculopathy. Spine, 31(5), 598-602.
Cleland, J. A., Whitman, J. M., Fritz, J. M., & Palmer, J. A. (2005). Manual physical therapy, cervical traction, and strengthening exercises in patients with cervical radiculopathy: a case series. Journal of Orthopaedic & Sports Physical Therapy, 35(12), 802-811.
Corey, D. L., & Comeau, D. (2014). Cervical radiculopathy. Medical Clinics of North America, 98(4), 791-799.
Costello, M. (2008). Treatment of a patient with cervical radiculopathy using thoracic spine thrust manipulation, soft tissue mobilization, and exercise.Journal of Manual & Manipulative Therapy, 16(3), 129-135.
Engquist, M., Löfgren, H., Öberg, B., Holtz, A., Peolsson, A., Söderlund, A., ... & Lind, B. (2013). Surgery versus nonsurgical treatment of cervical radiculopathy: a prospective, randomized study comparing surgery plus physiotherapy with physiotherapy alone with a 2-year follow-up. Spine,38(20), 1715-1722.
Grotle, M., & Hagen, K. B. (2014). Surgery for cervical radiculopathy followed by physiotherapy may resolve symptoms faster than physiotherapy alone, but with few differences at two years. Journal of physiotherapy, 60(2), 109.
Kuijper, B., Tans, J. T. J., Schimsheimer, R. J., Van Der Kallen, B. F. W., Beelen, A., Nollet, F., & De Visser, M. (2009). Degenerative cervical radiculopathy: diagnosis and conservative treatment. A review. European Journal of Neurology, 16(1), 15-20.
Leininger, B., Bronfort, G., Evans, R., & Reiter, T. (2011). Spinal manipulation or mobilization for radiculopathy: a systematic review. Physical medicine and rehabilitation clinics of North America, 22(1), 105-125.
Raney, N. H., Petersen, E. J., Smith, T. A., Cowan, J. E., Rendeiro, D. G., Deyle, G. D., & Childs, J. D. (2009). Development of a clinical prediction rule to identify patients with neck pain likely to benefit from cervical traction and exercise. European Spine Journal, 18(3), 382-391.
Swezey RL, Swezey AM, Warner K. Efficacy of home cervical traction therapy. Am J Phys Med Rehabil. Jan-Feb 1999;78(1):30–32.
Valtonen EJ, Kiuru E. Cervical traction as a therapeutic tool. A clinical anlaysis based on 212 patients. Scand J Rehabil Med. 1970;2(1):29–36
van der Heijden GJ, Beurskens AJ, Koes BW, Assendelft WJ, de Vet HC, Bouter LM. The efficacy of traction for back and neck pain: a systematic, blinded review of randomized clinical trial methods. Phys Ther. Feb 1995;75(2):93–104.
Wainner, R. S., Fritz, J. M., Irrgang, J. J., Boninger, M. L., Delitto, A., & Allison, S. (2003). Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy.Spine, 28(1), 52-62.
Waldrop, M. A. (2006). Diagnosis and treatment of cervical radiculopathy using a clinical prediction rule and a multimodal intervention approach: a case series. Journal of Orthopaedic & Sports Physical Therapy, 36(3), 152-159.
Wong AM, Lee MY, Chang WH, Tang FT. Clinical trial of a cervical traction modality with electromyographic biofeedback. Am J Phys Med Rehabil. Jan-Feb 1997;76(1):19–25.