Contralateral Knee Extension - a New Advance in Slump Test
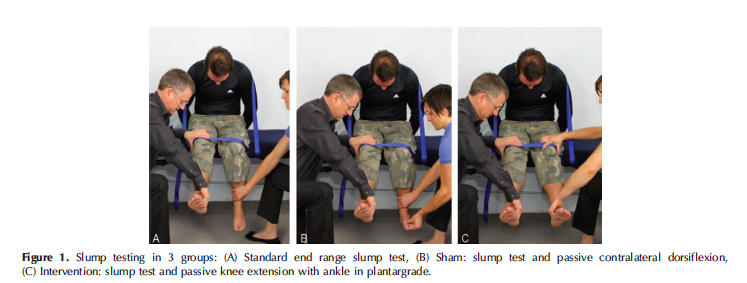
This year Shacklock et al (2016) published a fantastic study exploring the impact that a contralateral knee extension has on asymptomatic subjects during the slump test (see original paper here). The purpose of the study was to understand what the normal response is in asymptomatic subjects when this additional movement is performed.
The results of this study help us to understand further the mechanics of movement of the lumbar nerve roots during neurodynamic movements/tests and provide clinicians with new information about how to interpret the response a patient feels during the slump test.
I’m sure we are all familiar with performing the slump test in clinical practice, as it is indicated for patients with both lower back and neck pain. Over the past years I have learnt further details about how to perform this test reliably and consistently and the main purpose of this blog is to:
- Discuss what the normal test procedures is and what the normal response is in asymptomatic patients.
- Share the new findings associated with the addition of contralateral knee extension at the end of the movement.
Slump test - a neurodynamic assessment
Use of the slump test is indicated for pain in any area of the body, but is most commonly used in the assessment of lower back pain. It falls under the category of neurodynamic assessment. Maitland (2005) emphasises that the slump test is applicable to both lumbar and cervical spine disorders and should be included in the musculoskeletal assessment. For the lumbar spine specifically, the slump test is often used to test the mechanics of lumbar neural tissues and identify lumbar disc herniations.
You may also wonder why you perform both lumbar flexion AROM and a slump test when both produce spinal flexion. The answer is that...
"If forward flexion is restricted, it may be that the intervertebral joints are stiff or it may be that there is loss of movement of the structures in the canal or foramen. The tests that can be applied to move the structures in the vertebral canal without also moving the intervertebral joints are few in number" (Maitland, et al., 2005, p. 140).
Performing the slump test
Maitland (2005) & Shacklock (2005) instruct the process of a slump test as:
- Have the patient sit on the edge of the couch with the back of their knees touching the edge of the couch. Ask for resting pain/symptoms.
- Hands resting on the couch behind the patient’s back.
- Instruct the patient to slump through their upper and lower back (without flexing the cervical spine) and the therapist applies a gentle over-pressure (not to end of range). A good instruction is to ask the patient to slump their shoulders to hips and drop straight down. The aim is full lumbar and thoracic flexion. Assess for any change of symptoms.
- Instruct the patient to tuck their chin to chest as they look down and a firm overpressure is applied by the therapist to maintain cervical/thoracic/lumbar position. Assess for any change in symptoms.
- Instruct the patient to extend their knee as far as possible and note the range of symptoms or pain response. Ask "Is that your pain?".
- The end position is sustained while neck flexion is released and the change in pain response is noted. Also, if the patient is unable to achieve full knee extension, then once neck flexion is released, ask the patient to try extend their knee further.
- Ankle dorsiflexion can be added before or after knee extension to increase the stretch and assist with structural differentiation.
- If firmer over-pressure is required, repeat the test in long sitting.
- Therapists should also decide, based on the patient history, if over-pressure is appropriate at all. "The therapist must take into account specific information, such as irritability, sensitivity, latency and contraindications" (Shacklock, 2005, p. 143).
Below is the sequence I use for the slump test. If the patient is sitting on the end of the plinth as seen below then you can stand beside your patient. If they are sitting in the middle of the plinth you will need to perch on the table next to them in order to position yourself correctly to sustained the thoracic position and help your client maintain their slump while they move their cervical spine.
Most importantly remember to ask for the pain response, pain location and relationship to the patient's problem. Then ensure to assess the change in pain response with release of cervical flexion.
Positive response: Both the increased knee extension range and reduction in symptoms with release of cervical flexion would implicate dural pain-sensitised structures over hamstring muscle extensibility, as the limiting factor to knee extension range of movement.
Normal response (Maitland, 2005; Shacklock, 2005):
- Mid thoracic (T9/10) pain/discomfort during thoracic and lumbar flexion.
- A pain free lack of 30 degrees of knee extension can be normal.
- Stretching in the posterior thigh and knee, extending into the calf.
- Ankle dorsiflexion increases the posterior thigh/knee pain.
- Reduction of symptoms with release of cervical flexion.
A word of caution…
Maitland alerts therapists to the often-unpredictable response that patients with pain-sensitive canal structures and neural structures may have to the slump test or slump exercises. "Therefore, when the slump test is used as a technique, care must be taken on the first day and assessment over 24 hours is then necessary to determine whether the strength of the technique needs to be changed. If it is performed vigorously, an interval of 2-3 days should be left between treatments for soreness to settle so as to make accurate reassessment possible to determine how much has been gained" (2005, p. 149).
Updates in our understanding of a 'normal response'
What do we know is happening during the slump test?
Shacklock and his team have been studying the movement of neural tissues for many years in the hope of understanding the mechanism behind these responses. Coming back to the study above, Shacklock et al (2016) looked at the change in pain (measured on the numerical rating of pain scale) when the contralateral knee was extended.
What they found is the in every patient within the intervention group, the 'evoked sensation' in the test leg was reduced when the other knee was extended.
In fact, the change in sensation following contralateral knee extension in the intervention group was on average 3.8 on the numerical rating scale (Shacklock, et al., 2016, p. E208).
(Shacklock, et al., 2016., E207)
First they measured the physical impact of this movement and then they studied it on cadavers. The second part of the study was to test the movement of lumbar neural tissues with mechanical traction in cadavers.
What they found is that when a mechanical traction was applied to the nerve root (in this case L5) in a caudal direction, all neural tissues on the opposite side become looser (Shacklock, et al., 2016, p. E208).
(Shacklock, et al., 2016, p. E208)
A video of this movement is available directly from the article under supplementary digital images in the article itself or you can try view them on this link.
How does this translate to clinical practice?
On of the main take home messages from this article about the slump test is that moving the opposite side changes tension in the lumbar neural tissues.
When contralateral knee extension is applied there is likely a caudal traction force on the lumbar nerve roots resulting in reduced nerve root pressure. This helps us to understand a little more why some patients with sciatica can experience temporary relief in their symptoms performing this test. While it may look like extending both legs is a stronger slump test, if performed in the correct sequence, it may in fact be reducing the pressure?!
Clinically I have seen this work and often give this movement as a HEP for reducing pain. But, understanding the mechanism as to how this movement works has not until recent times been fully understood.
How do we know that it isn't due to hamstring muscle tension?
One confounding factor that could result in reduction of symptoms is the relaxation of soft tissue structures in the thigh. When the evoked sensation in the testing leg changes with a release of cervical flexion and there is no change in myoelectric activity in the hamstrings, the change is thought to be associated with lumbar neural tissues (Shacklock, et al., 2016). Based on this thinking the authors designed the study to control for any soft tissue changes by also having a control and sham group.
Is this just in asymptomatic subjects?
The first stage of this research is to improve our understanding of what normally happens during these movements in asymptomatic individuals. From here researchers can continue to study and understand the abnormal response too. You've probably seen it before and just not entirely understood what you were looking at.
I first came across the idea of movement in the spinal cord when I was taught the “crossed SLR sign”. The crossed straight leg raise is when a patient with LBP performs an ALSR test and lifting the contralateral leg produces increased pain. I was taught this when I first started practicing and have seen it many times before.
Initially I just looked for this sign but didn't fully understand what it meant. Now I know that the crossed SLR sign is an indicator of lumbar disc herniation and these patient's were generally slower to recover or more tricky to manage.
The results from this study help me to understand and conceptualise the movement of lumbar neural tissues and why this might be the case. Although further research is still required to provide a sound explanation for these outcomes, there is growing evidence that neurodynamic tests such as the slump test provide us with invaluable information of the neural mechanics of our patients. Understanding more about how the neural tissue move in response to limb movements will help us to develop better treatments and home-exercises for our patients with back pain.
Sian ;)
Follow neurodynamic updates from Michael Shacklock directly via Research Gate and access the original paper here.
For variations in the slump test and passive straight leg raise test refer to Maitland's book Vertebral Manipulation, Shacklock's book Clinical Neurodynamics, and Butler’s book The Neurodynamic techniques (Butler, 2005; Hengeveld & Banks, 2005; Shacklock, 2005).
References:
Hengeveld, E., & Banks, K. (2005). Maitland's peripheral manipulation: Elsevier/Butterworth Heinemann.
Shacklock, M., Yee, B., Van Hoof, T., Foley, R., Boddie, K., Lacey, E., ... & Airaksinen, O. (2016). Slump Test: Effect of Contralateral Knee Extension on Response Sensations in Asymptomatic Subjects and Cadaver Study. Spine,41(4), E205-E210.
Shacklock, M. O. (2005). Clinical neurodynamics: a new system of musculoskeletal treatment: Elsevier Health Sciences.