A Complex Case of Shoulder Multidirectional Instability in A Patient with hypermobile Ehlers-Danlos Syndrome and Post-Traumatic Stress Disorder
As part of the specialisation program, I was required to write a case study on a complex patient who required “specialist” management. It challenged me to consider all aspects of a patient’s presentation, without biasing any one area. It definitely showed me the multitude of contributors to a patient’s pain experience, the necessity for accurate diagnosis and the difficulties when working with limited resources.
Lola
This complex case report describes ‘Lola’, a 53-year-old Aboriginal woman presenting with severe, disabling shoulder pain. Her case is presented to highlight the complications of undiagnosed hEDS and issues associated with pain management for Aboriginal Australians in a rural setting.
Ehlers-Danlos syndromes (EDS) are a group of hereditary connective tissue disorders characterised by soft tissue laxity, joint hypermobility and tissue fragility (Benistan & Martinez 2019).
The 2017 International Classification includes 13 subtypes, with hypermobile Ehlers-Danlos syndrome (hEDS) accounting for 80 per cent of cases (Malfait et al 2017). While 12 subtypes are diagnosed genetically, hEDS is diagnosed clinically based on strict diagnostic criteria (Malfait et al 2017).
Prevalence is estimated at two per cent, affecting more females than males (Reychler et al). Individuals are generally younger and have longer pain duration than other chronic pain conditions (Molander et al 2020).
Widespread pain and fatigue are common, causing severe disability and altered quality of life (Benistan & Martinez 2019). Underlying pain mechanisms are poorly understood, with nociceptive and neuropathic pain (Benistan & Gillas 2020), deconditioning and central sensitisation likely contributing factors. Recent evidence implicates deficits in endogenous pain inhibitory control, indicated by abnormal conditioned pain modulation (Leone et al 2020).
Fatigue, widespread pain and fear of injury are reported as barriers to exercise (Simmonds et al 2019), and impacting on their workplace. Individuals reported taking copious sick leave, reducing work hours and working through pain to avoid judgement (Bennet et al 2021).
Kinesiophobia is strongly associated with hEDS, with repetitive musculoskeletal trauma leading to avoidance behaviours and deconditioning (Celletti et al 2013).
In those with hEDS, 69 per cent have depression and 73 per cent have anxiety, with a very high rate of suicide attempts observed (Benistan & Martinez 2019). Patients report being stigmatised, ignored or belittled by medical professionals and receiving a lack of psychological support (Bennet et al 2021).
Aboriginal and Torres Strait Islander Australians have 1.5 times greater risk of rheumatoid conditions, and 1.4 times higher burden of musculoskeletal pain, compared to non-Aboriginal Australians (Lin 2020). Aboriginal Australians have a higher prevalence of anxiety and depression, and psychosocial risk factors including psychological distress, financial stress and low income and employment, compared to non-Aboriginal Australians (Marwick et al 2014).
History
Lola presented with a four-month history of disabling left shoulder pain. She believed she had ‘torn the tendon off the bone’ during a student-led gym class, which she was attending for fibromyalgia and anxiety.
Six months previously, she was referred to a rheumatologist, who diagnosed Lola with fibromyalgia and prescribed 25 milligrams amitriptyline and 15 milligrams meloxicam daily. She was instructed to complete a weekly gym program to assist with management.
The rheumatologist was concerned she had ankylosing spondylitis, so spinal x-rays and blood tests were completed. These were negative, so Lola was diagnosed with ‘piriformis syndrome’ and told to ‘go home and look it up’. Lola was relieved with her piriformis syndrome diagnosis, as having ankylosing spondylitis meant she would ‘end up in a wheelchair’.
The onset of her ‘piriformis syndrome’ eight years earlier corresponded to leaving an abusive relationship, being homeless for two weeks and living in her car with her son. At this same time, her mother had died in a “very traumatic” palliative care situation. Lola reported being sexually abused as a child by two perpetrators over multiple years, and still had regular flashbacks. Lola disclosed this was the first she had spoken to medical professionals about her abusive history.
She also reported nine years of lumbar pain (diagnosed as arthritis), bilateral lateral hip pain, jaw pain and two previous patellar dislocations. During childhood, she habitually self-dislocated both shoulders. Lola reported extreme fatigue, light headedness on changing positions, followed a strict FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides and polyols) diet for gut intolerances and was menopausal. She had previously undergone five surgeries for a deviated septum and sinus pathologies.
Three months prior to the initial assessment, Lola was diagnosed with depression by her general practitioner (GP), after being unable to get out of bed for five days following an exacerbation of her left shoulder pain. Lola was advised to continue exercising and administering Amitriptyline.
Lola was highly distressed to be seeing another medical professional, reporting waking ten times the previous night as she was ‘anxious to say everything right’.
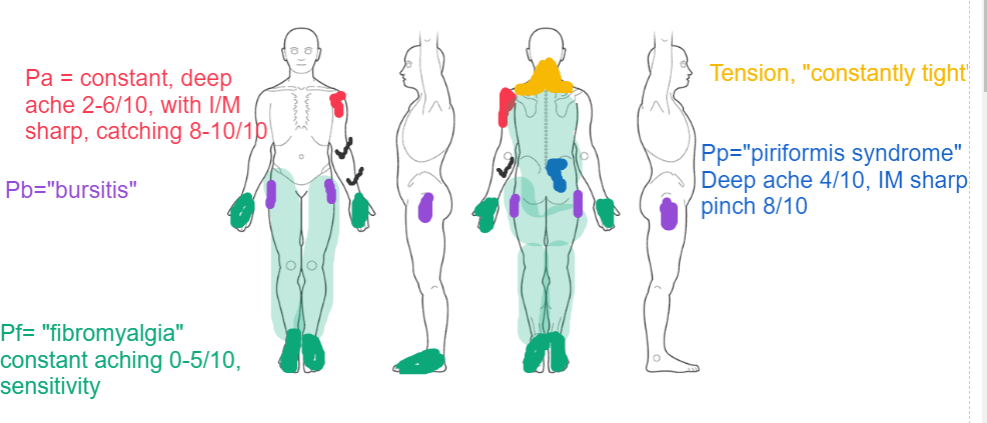
Figure 1. Body Chart at Initial Assessment.
Lola’s presenting complaint (left shoulder pain) was aggravated with any sudden or unexpected shoulder movements, and any elevation greater than 50 -degrees. Lola was cautious while changing sheets on the bed, putting clothes on the clothesline and dressing. When sneezing or yawning, Lola would hold her shoulder for support to reduce symptoms.
Lola reported regular left shoulder clicking, and up to ten daily episodes of severe, sharp catching pain on sudden movements. She would hold her shoulder and breathe through pursed lips for up to three minutes, until the pain subsided. Lola subsequently avoided any overhead movements, lifting any object greater than 500 grams and using her left arm for any self-care activities.
Lola described a three-year history of progressive bilateral shoulder pain, which she understood as being ‘bursitis’ and ‘tendonitis’, diagnosed on ultrasound. Although no specific incident could be recalled, Lola was adamant adding bent-over row exercises initiated her shoulder exacerbation four months earlier.
She had constant neck tension, worse on the left side, which had increased since the gym incident. She experienced no paraesthesia or headaches, but reported sensitivity to fluorescent lights.
Lola had very poor sleep, reporting waking 10-15 times per night due to both left shoulder and right ‘piriformis’ pain. She would sleep for four to five hours of broken sleep, further disrupted with intermittent flashbacks of previously mentioned traumatic events.
On waking, Lola experienced 60 minutes of severe ‘fibromyalgia pain’ in her hands and feet, with extreme difficulty walking due to feet sensitivity. This slowly reduced from 8/10 on the numerical rating scale (NRS) to 3/10 within 30 minutes. She reported severe exhaustion, never feeling fully rested.
Lola lived with her sixteen-year-old son and sold jewellery at markets for 15 hours per week to fulfil requirements for Centrelink assistance. Her pain was affecting her ability to complete this time requirement, with Lola highly concerned about ‘keeping a roof overhead’. She had two supportive friends, but no close family assistance.
Her primary goals were to reduce her shoulder pain on overhead movements and fulfil her weekly time commitment to maintain Centrelink allowance.
Clinical Reasoning
Multiple psychosocial and lifestyle considerations were identified following subjective questioning (Mitchell et al 2018).
Psychosocial Contributors
Social Factors - high
· Distress surrounding her financial situation, ability to fulfil Centrelink employment criteria and potential homelessness
· Poor social support
Affective Factors – high
· Depression, anxiety and symptoms consistent with post-traumatic stress disorder (PTSD)
Cognitive Factors – high
· Strong biomedical beliefs, reliance on radiology, reinforced by medical practitioners
· Avoidant behaviours were yet unclear if helpful or unhelpful
Lifestyle Considerations - moderate
· Poor sleep
· Deconditioning
· FODMAP diet and regular gentle exercise appeared protective for pain (Marum et al 2016)
Whole Person Considerations - high
· High previous life stress & childhood trauma
· Fibromyalgia
· Suspected Ehlers-Danlos syndrome
· Menopause
A shortened physical examination was performed, for concern that prolonged manual testing would heighten patient distress and reinforce a biomedical approach.
Physical Examination
Lola appeared visibly distressed, with an apical breathing pattern and holding her left forearm braced across her abdomen. All movements appeared guarded and apprehensive. Undressing induced breath-holding and cautious movement of her left arm.
Resting standing posture showed downwardly rotated scapulae bilaterally, with her left shoulder in anterior scapula tilt and left forearm braced across her abdomen.
Left shoulder movements were limited by pain, which were improved with scapular upward rotation assistance and posterior glenohumeral support. Instability tests were positive bilaterally, with left sulcus sign test reproducing 5/10 shoulder pain and severe distress, evidenced by shrieking, holding her left shoulder and undertaking ‘meditative’ deep breathing.
Left shoulder horizontal adduction reproduced posterior glenohumeral pain and moderate apprehension. Left shoulder Apprehension Test reproduced breath-holding and strong guarding into abduction and external rotation. Providing concurrent anterior and posterior glenohumeral joint support (modified Jobes Relocation Test) reduced apprehension, increased shoulder range of motion, and visibly normalised her breathing pattern. Anterior and posterior shoulder draw tests appeared moderately lax bilaterally in 30-degree abduction, with left reproducing severe apprehension.
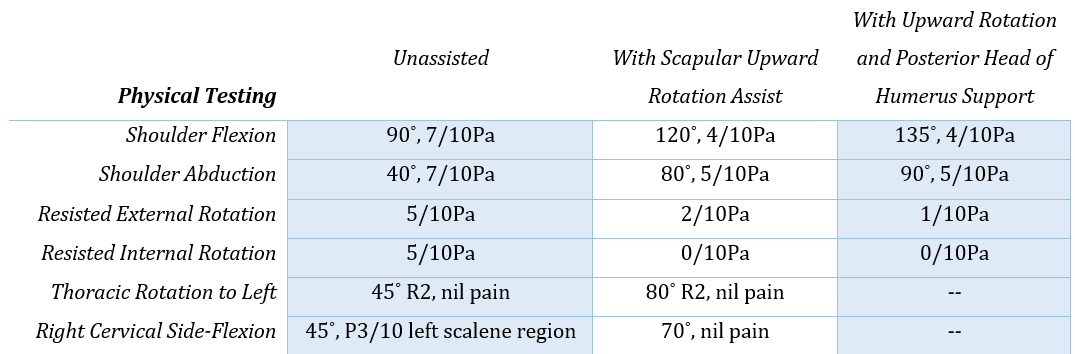
Thoracic and cervical range of motion were limited (see Table 1). Isometric resisted shoulder internal and external rotation were provocative. All movements were improved with scapular upward rotation assistance and glenohumeral support (see Table 1).
Table 1. Key Physical Findings on Initial Assessment.
Scapular upward rotation shrugs in 30˚ shoulder abduction were limited to 6 repetitions (left) and 9 repetitions (right) before fatigue. Isometric prone scapular hold in 30˚ shoulder abduction fatigued at 7 seconds on the left, and 11 seconds on right.
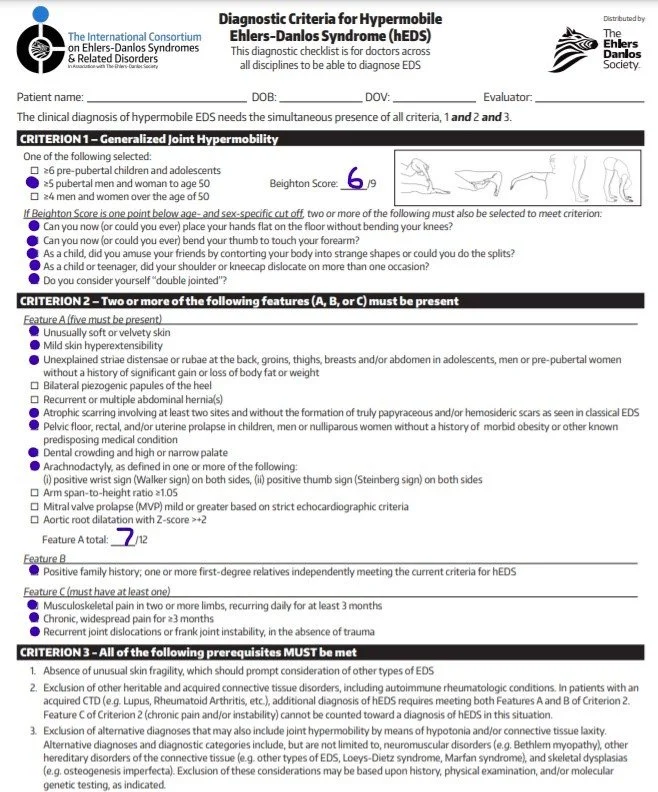
Hypermobility testing was positive with a Beighton Score of 6/9, highly specific for hypermobility in females 40-59 years old (Singh et al 2017). Her hypermobility, and extensive multi-system medical history, prompted additional testing for Ehlers-Danlos syndrome.
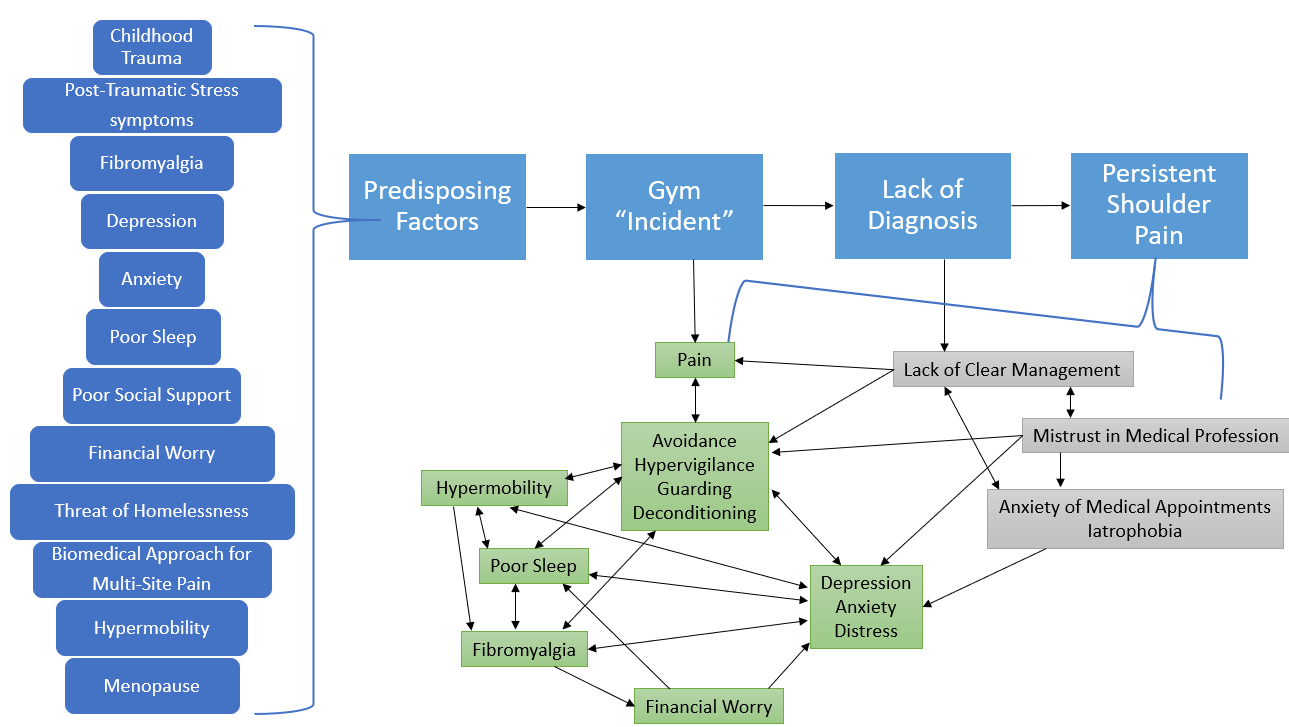
Lola fulfilled the diagnostic criteria for hEDS (see Image 4).
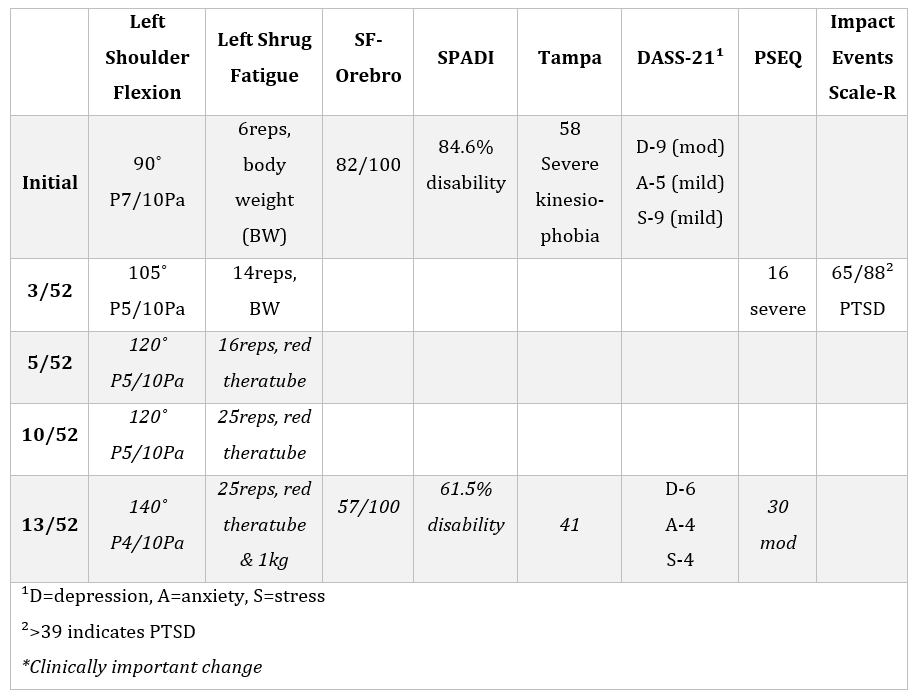
Self-reported outcome measures were administered over multiple sessions, showing high scores on short-form Orebro, Shoulder Pain and Disability Index (SPADI), Tampa scale for Kinesiophobia and Pain Self Efficacy Questionnaire (PSEQ) (see Table 2).
Table 2. Key Assessment Measures.
Diagnosis
Lola was diagnosed with left shoulder multidirectional instability (Warby et al 2018). She fulfilled the criteria of hEDS (Malfait 2017) (see figure 4), and exceeded cut-off limits for PTSD on Impact of Events scale (IES-R) (Creamer et al 2003). She displayed multiple psychosocial and lifestyle contributors, as previously mentioned (see Figure 2).
Figure 2. Key Contributing Factors and Relationships in Lola’s Shoulder Pain Experience.
Management
Initial management focused on reducing left shoulder pain on movement, to facilitate therapeutic alliance (Kinney et al 2020) and develop patient confidence, whilst also addressing psychosocial and lifestyle contributors.
Scapular upward rotation and glenohumeral support was actively achieved with a shoulder shrug (see Figure 3a), and shrug combined with shoulder row (see Figure 3b), using a Theraband for proprioceptive feedback and resistance (Warby et al 2018, Watson et al 2018).
Shoulder flexion improved to 130-degrees with 4/10 pain, immediately following exercises; the patient then volunteered to perform these exercises three times daily.
Shoulder taping, supporting scapular upward rotation and glenohumeral support, reduced pain on shoulder flexion to 2/10 on NRS, and improved apprehension on horizontal adduction by 80 per cent (see Figure 3c).
Figure 3. Exercise Prescription and Taping Technique.
An explanation of her pain was provided using a flow chart (similar to Figure 2). Using the flow chart to guide shared decision-making, a collaborative plan was implemented to involve other service providers (Frantsve & Kerns 2007).
The diagnosis of hypermobile Ehlers-Danlos syndrome was discussed (Benistan & Martinez 2019, see Figure 4), employing a clinical yarning style of communication to facilitate therapeutic alliance (Lin et al 2016, Babatunde et al 2017).
Figure 4. Diagnostic Criteria for hypermobile Ehlers-Danlos Syndrome (Malfait et al 2017).
Communication with her general practitioner initiated a medication review with a pain physician, referral to social work for finance assistance, psychology referral and rheumatology referral for Ehlers-Danlos syndrome confirmation.
The patient was encouraged to continue her low FODMAP diet to manage her hEDS and fibromyalgia (Marum et al 2016, Fragkos et al 2019), with early evidence indicating this diet has a greater effect on irritable bowel symptoms in those with joint hypermobility syndrome, than those without. This validated Lola’s previous self-management strategies and own learned experience of her triggers (Bennett et al 2019).
Her weekly exercise program was modified to meet fibromyalgia and persistent pain recommendations, while addressing fear of pain and further injury (Simmond et al 2019). Weighted arm activities were ceased, with cardiovascular exercise modified to moderate-intensity, low impact movements (elliptical trainer and upright bike) (Busch et al 2013).
Progress in Five Sessions (13 Weeks)
Following initial assessment, Lola did not get out of bed for five days due to drastic increases in pain and severe flashbacks of childhood trauma. She reported increased awareness of the relationship between her emotional state and her pain.
Revision with a pain physician, eight weeks after initial assessment, prompted the addition of duloxetine 60 milligrams to address depression and central pain mechanisms (Finnerup et al 2015).
She now wakes one or two times per night, reporting much improved sleep and quality of life. Her morning ‘fibromyalgia’ pain has resolved.
Psychological referral took three months, with only one session attended at time of writing. Rheumatological revision had a five-month wait and has not yet occurred.
Physiotherapy management is continuing, focusing on progressing shoulder rehabilitation (Watson et al 2018), and facilitating therapeutic alliance and patient advocacy (Simmonds et al 2019, Bennett et al 2021).
Lola is now on a disability pension and continues to work 15 hours weekly. She reports relief about having the hEDS diagnosis, as it validates her pain experience, justifies her extensive medical history, and provides guidance for management.
Discussion
Management
To address the patient’s goals, management was targeted on addressing the shoulder nociceptive pathology, in the context of a persistent pain presentation. Current guidelines support an interdisciplinary management strategy to address persistent pain, specifically including physical, psychological, social engagement and nutrition intervention (Painaustralia 2021).
Protective factors for this patient include her low FODMAP diet (Marum et al 2016, Fragkos et al 2019), her dedication to exercise (Reychler et al 2021, Simmonds et al 2019) and her avoidance of opioid medication. Generally, those with EDS are reported to administer almost double the opioid dosage of controls, leading to opioid induced hyperalgesia and dependency (Schubart et al 2019).
While definitive pharmacological recommendations for hEDS are lacking, pharmacological management for fibromyalgia recommends duloxetine for severe pain and amitriptyline for severe sleep problems (Macfarlane et al 2017), which may impact on depression and anxiety (Finnerup et al 2015).
Initial physiotherapy management focused on addressing the peripheral nociceptive shoulder pain, as a means of gaining patient confidence and building therapeutic alliance. Sustained mechanical nociception is associated with reduced inhibitory control (Leone et al 2020). Addressing this modifiable stimulus provided an opportunity to build trust and address psychosocial and lifestyle contributors (Bennett et al 2021), while downregulating the barrage of afferent input.
Asymmetrical proprioception has been identified in hEDS (Benistan & Martinez 2019), with a relationship between proprioceptive improvements and pain reduction (Revivo et al 2019). Taping was used to provide additional proprioceptive feedback, perceived joint support and augment improvements achieved with the rehabilitation program.
Addressing deficits in scapular upward rotation, external rotation and posterior head of humerus control has been shown to be effective in managing multidirectional shoulder instability (Warby et al 2018, Watson et al 2018). This was further evidenced with large improvements in pain with manual upward rotation assistance and glenohumeral support, and weakness and poor endurance of upper trapezius.
Providing external rotation strength is recommended to increase the posterior scapular support (Watson et al 2018). In patients with Ehlers-Danlos, external rotation is proposed to increase the translation of the humeral head, therefore external rotation in early rehabilitation was avoided (Spanhove et al 2020). This will be added to the patient’s program once sufficient scapular strength and sagittal plane control has been achieved (Watson et al 2018).
The same study proposed holding dumbbells increases inferior humeral translation (Spanhove et al 2020), so dumbbells were replaced with Therabands until the patient could hold one kilogram without a positive sulcus sign.
Challenges and Opportunities
Patients with Ehlers-Danlos often experience misdiagnosis, most commonly being diagnosed with fibromyalgia (26 per cent), psychological diseases (21 per cent) and rheumatological joint disease (16 per cent), with diagnosis often occurring 14-24 years following initial symptoms (Benistan & Mertinez 2019).
In this case, a fibromyalgia diagnosis was provided eight years after symptoms developed, while post-traumatic stress disorder and Ehlers-Danlos syndrome are yet to be definitively diagnosed. Depression was diagnosed but no active management strategy was provided. These multiple diagnoses, combined with a lack of integrated multidisciplinary care, added to the patient’s distress and mistrust in medical management.
Care was further delayed due to lack of specialist intervention available in rural areas. Psychology referral took three months, while rheumatology will take five months. This may be due to the current Covid-19 climate, with rural outreach specialist consultations being cancelled, due to difficulties maintaining a rural health workforce or high demand on resources.
A unique opportunity exists to better integrate rural demands with urban resources, utilising technology to allow earlier healthcare referrals to appropriate professionals.
Conclusion
This case highlights the important role of physiotherapists in identifying hEDS and the multitude of contributing factors to persistent pain presentations, particularly in Indigenous Australians already at greater risk of chronic disease. A strong therapeutic alliance, with shared decision making, and building a multidisciplinary team, allowed the patient to actively participate in her own management, improving her quality of life and disability.
Alicia Rayner
References
Babatunde, F., MacDermid, J., & MacIntyre, N. (2017). Characteristics of therapeutic alliance in musculoskeletal physiotherapy and occupational therapy practice: a scoping review of the literature (vol 17, 375, 2017). Bmc Health Services Research, 17.
Benistan, K., & Gillas, F. (2020). Pain in Ehlers-Danlos syndromes. Joint Bone Spine, 87(3), 199-201. doi:10.1016/j.jbspin.2019.09.011
Benistan, K., & Martinez, V. (2019). Pain in hypermobile Ehlers-Danlos syndrome: New insights using new criteria. American Journal of Medical Genetics Part A, 179(7), 1226-1234. doi:10.1002/ajmg.a.61175
Bennett, S. E., Walsh, N., Moss, T., & Palmer, S. (2019). The lived experience of Joint Hypermobility and Ehlers-Danlos Syndromes: a systematic review and thematic synthesis. Physical Therapy Reviews, 24(1-2), 12-28. doi:10.1080/10833196.2019.1590674
Bennett, S. E., Walsh, N., Moss, T., & Palmer, S. (2021). Understanding the psychosocial impact of joint hypermobility syndrome and Ehlers-Danlos syndrome hypermobility type: a qualitative interview study. Disability and Rehabilitation, 43(6), 795-804. doi:10.1080/09638288.2019.1641848
Busch, A. J., Webber, S. C., Richards, R. S., Bidonde, J., Schachter, C. L., Schafer, L. A., . . . Overend, T. J. (2013). Resistance exercise training for fibromyalgia. Cochrane Database of Systematic Reviews(12). doi:10.1002/14651858.cd010884
Celletti, C., Castori, M., La Torre, G., & Camerota, F. (2013). Evaluation of Kinesiophobia and Its Correlations with Pain and Fatigue in Joint Hypermobility Syndrome/Ehlers-Danlos Syndrome Hypermobility Type. Biomed Research International, 2013. doi:10.1155/2013/580460
Creamer, M., Bell, R., & Failla, S. (2003). Psychometric properties of the Impact of Event Scale - Revised. Behaviour Research and Therapy, 41(12), 1489-1496. doi:10.1016/j.brat.2003.07.010
Finnerup, N. B., Attal, N., Haroutounian, S., McNicol, E., Baron, R., Dworkin, R. H., . . . Wallace, M. (2015). Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurology, 14(2), 162-173.
Fragkos, K. C., Keetarut, K., Cox, A., Eady, J., Emmanuel, A. V., & Zarate-Lopez, N. (2019). Joint Hypermobility Syndrome Affects Response to a Low Fermentable Oligosaccharide, Disaccharide, Monosaccharide and Polyol Diet in Irritable Bowel Syndrome Patients: A Retrospective Study. Gastroenterology Research, 12(1), 27-36. doi:10.14740/gr1133
Frantsve, L. M. E., & Kerns, R. D. (2007). Patient-provider interactions in the management of chronic pain: Current findings within the context of shared medical decision making. Pain Medicine, 8(1), 25-35. doi:10.1111/j.1526-4637.2007.00250.x
Kinney, M., Seider, J., Beaty, A. F., Coughlin, K., Dyal, M., & Clewley, D. (2020). The impact of therapeutic alliance in physical therapy for chronic musculoskeletal pain: A systematic review of the literature. Physiotherapy Theory and Practice, 36(8), 886-898. doi:10.1080/09593985.2018.1516015
Leone, C. M., Celletti, C., Gaudiano, G., Puglisi, P. A., Fasolino, A., Cruccu, G., . . . Truini, A. (2020). Pain due to Ehlers-Danlos Syndrome Is Associated with Deficit of the Endogenous Pain Inhibitory Control. Pain Medicine, 21(9), 1929-1935. doi:10.1093/pm/pnaa038
Lin, I., Coffin, J., Bullen, J., & Barnabe, C. (2020). Opportunities and challenges for physical rehabilitation with indigenous populations. Pain Rep, 5(5), e838.
Lin, I., Green, C., & Bessarab, D. (2016). "Yarn with me': applying clinical yarning to improve clinician-patient communication in Aboriginal health care. Australian Journal of Primary Health, 22(5), 377-382. doi:10.1071/py16051
Macfarlane, G. J., Kronisch, C., Atzeni, F., Hauser, W., Choy, E. H., Amris, K., . . . Jones, G. T. (2017). EULAR recommendations for management of fibromyalgia. Annals of the Rheumatic Diseases, 76(12). doi:10.1136/annrheumdis-2017-211587
Malfait, F., Francomano, C., Byers, P., Belmont, J., Berglund, B., Black, J., . . . Tinkle, B. (2017). The 2017 International Classification of the Ehlers-Danlos Syndromes. American Journal of Medical Genetics Part C-Seminars in Medical Genetics, 175(1), 8-26.
Markwick, A., Ansari, Z., Sullivan, M., Parsons, L., & McNeil, J. (2014). Inequalities in the social determinants of health of Aboriginal and Torres Strait Islander People: a cross-sectional population-based study in the Australian state of Victoria. International Journal for Equity in Health, 13. doi:10.1186/s12939-014-0091-5
Marum, A. P., Moreira, C., Saraiva, F., Tomas-Carus, P., & Sousa-Guerreiro, C. (2016). A low fermentable oligo-di-mono saccharides and polyols (FODMAP) diet reduced pain and improved daily life in fibromyalgia patients. Scandinavian Journal of Pain, 13, 166-172. doi:10.1016/j.sjpain.2016.07.004
Mitchell, T., Beales, D., Slater, H., & O'Sullivan, P. (2018). Musculoskeletal Clinical Translation Framework: From Knowing to Doing (eBook).
Molander, P., Novo, M., Hallstam, A., Lofgren, M., Stalnacke, B. M., & Gerdle, B. (2020). Ehlers-Danlos Syndrome and Hypermobility Syndrome Compared with Other Common Chronic Pain Diagnoses-A Study from the Swedish Quality Registry for Pain Rehabilitation. Journal of Clinical Medicine, 9(7). doi:10.3390/jcm9072143
Painaustralia. (2021). National Strategic Action Plan for Pain Management.
Revivo, G., Amstutz, D. K., Gagnon, C. M., & McCormick, Z. L. (2019). Interdisciplinary Pain Management Improves Pain and Function in Pediatric Patients with Chronic Pain Associated with Joint Hypermobility Syndrome. Pm&R, 11(2), 150-157. doi:10.1016/j.pmrj.2018.06.018
Reychler, G., De Backer, M. M., Piraux, E., Poncin, W., & Caty, G. Physical therapy treatment of hypermobile Ehlers-Danlos syndrome: A systematic review. American Journal of Medical Genetics Part A. doi:10.1002/ajmg.a.62393
Schubart, J. R., Schilling, A., Schaefer, E., Bascom, R., & Francomano, C. (2019). Use of prescription opioid and other drugs among a cohort of persons with Ehlers-Danlos syndrome: A retrospective study. American Journal of Medical Genetics Part A, 179(3), 397-403. doi:10.1002/ajmg.a.61031
Simmonds, J. V., Herbland, A., Hakim, A., Ninis, N., Lever, W., Aziz, Q., & Cairns, M. (2019). Exercise beliefs and behaviours of individuals with Joint Hypermobility syndrome/Ehlers-Danlos syndrome - hypermobility type. Disability and Rehabilitation, 41(4), 445-455. doi:10.1080/09638288.2017.1398278
Singh, H., McKay, M., Baldwin, J., Nicholson, L., Chan, C., Burns, J., & Hiller, C. E. (2017). Beighton scores and cut-offs across the lifespan: cross-sectional study of an Australian population. Rheumatology, 56(11), 1857-1864.
Spanhove, V., De Wandele, I., Kjaer, B. H., Malfait, F., Vanderstukken, F., & Cools, A. (2020). The effect of five isometric exercises on glenohumeral translations in healthy subjects and patients with the hypermobility type of the ehlers-danlos syndrome (heds) or hypermobility spectrum disorder (hsd) with multidirectional shoulder instability: an observational study. Physiotherapy, 107, 11-18. doi:10.1016/j.physio.2019.06.010
Warby, S. A., Ford, J. J., Hahne, A. J., Watson, L., Balster, S., Lenssen, R., & Pizzari, T. (2018). Comparison of 2 Exercise Rehabilitation Programs for Multidirectional Instability of the Glenohumeral Joint: A Randomized Controlled Trial. American Journal of Sports Medicine, 46(1), 87-97. doi:10.1177/0363546517734508
Watson, L., Balster, S., Lenssen, R., Hoy, G., & Pizzari, T. (2018). The effects of a conservative rehabilitation program for multidirectional instability of the shoulder. Journal of Shoulder and Elbow Surgery, 27(1), 104-111. doi:10.1016/j.jse.2017.07.002