Blood flow restriction training - a personal reflection
My story & BFR
At the beginning for 2020, and 10 years after his first reconstruction, my husband fell whilst snow skiing and ruptured his ACL for the 3rd time. MRI scans in February 2020 also revealed a tear in the posterior horn of the lateral meniscus and a large chondral lesion on the medial femoral condyle. Third ACL reconstructions aren’t that common and require a highly individualized approach. Full lower limb XRAYS and knee MRIs were taken to carefully analyze the alignment of both my husband’s legs and the alignment of the current graft and tunnel. It was decided that the it wouldn’t be sensible to try a third reconstruction without changing the position and angle of the ACL graft. This would involve a two-staged surgery over several months.
The first surgery involved removing the previous hardware and perform a bone graft on the original tunnel using allograft tissue. Although he was allowed to WBAT following this surgery, it took well over 4 weeks before he could start to comfortably weight bear. Following surgery, a standard protocol was recommended by the surgeon for return to ADLs and stationary cycling, except that a protective brace was worn for all activity. Three months later the second surgery was performed. This included an ACLR with allograft, lateral meniscus posterior root repair and large chondral plug repair from a non-weight bearing portion of the femoral condyle. He was non weight bearing for almost seven weeks. Then he began his rehabilitation following a standard ACL protocol.
Not only was this a challenging recovery with extended time either non weight bearing or restricted weight bearing, but there were other significant contextual barriers that impacted his recovery.
The first – COVID-19, which for us meant no family support. Our original shelter-in-place order (in San Francisco) was announced one week after surgery.
The second – we live on a third-floor condo with no elevator access, which meant he was isolated inside until he could safely negotiate 54 stairs.
The third – I was pregnant and unfortunately, placed on bedrest from 27-34 weeks. So, for a short period of time my husband was on crutches and I was on bedrest with a 2.5 year old daughter to keep us company.
Being his 3rd reconstruction and 5th surgery, I’d say I know a fair amount about ACL recovery, but what I appreciate is that all this knowledge about rehabilitation is almost useless if you don’t have the social environment to support a recovery plan. Whilst this was an extremely challenging year for us, it lead me to develop greater empathy for how it feels to support someone recovering from surgery and social support and environmental factors that should be considered during the evaluation.
All of those contextual factors meant there was nearly no time to complete the desired recovery. We poured all our energy into making it through the day and being parents. We were fortunate enough to have in-home physical therapy 1-2 times a week. But once baby #2 arrived, all available time an energy went into the kids. And hopefully now you can imagine just how much atrophy would have occurred since the original injury in January. We knew what exercises were needed to build strength and regain function but finding the time felt nearly impossible. And this is what lead us to wonder – how can we optimize time and augment healing? This is what lead us to explore blood flow restriction training (BFR).
Blood flow restriction training
Blood flow restriction training, or BFR, is an emerging hot topic in Physiotherapy rehabilitation. Although it has been around since the 60’s, it really only came to the United States in 2014. Since that time there has been an explosion in research looking into its properties and clinical application. BFR combines low intensity exercises with blood flow restriction using a medical grade tourniquet to create strength and hypertrophy changes, increased bone density and increased aerobic capacity in the tissues. It is starting to gain a lot more popularity in the clinical world as the research accumulates supporting the use of BFR with low intensity exercise in patients where high intensity exercise may not be suitable/restricted such as osteoporosis, menopause, post-operative, tendon dysrepair, and the elderly (Loenneke, et al., 2012). In 2018, the APTA determined that the use of BFR therapy is part of the professional scope of practice for Physical Therapy.
Our understanding of BFR has evolved significantly and Physical Therapists can now offer patient-centered treatment programs using individualized occlusion pressures and exercise prescription. Everyone will need a different pressure, based on their limb size, muscle mass and adipose tissue, to achieve the occlusion pressure that results in metabolic accumulation. By occluding venous blood flow and reducing arterial blood blow, your muscles will receive less oxygen and during the exercises there will be a switch from using type I to type II muscle fibers. Using BFR we are able to create the same metabolic stress in the tissues that occurs during high intensity strength training. These cellular changes result in adaptations to muscle strength without the associated muscle damage that is caused by high intensity resistance training. BRF has a time and place in the rehab journey, especially when high intensity training can’t be achieved (Bradner, et al., 2019). This is great news for the patients that would benefit from strengthening but are unable to complete high intensity training. As more research is published it appears there is no argument that BFR is a powerful tool to gaining strength if you can only lift light weights. Below is a table demonstrating the metabolic and mechanical changes which occur with HIRT, BRF and LIRE and LIRE alone.
This table is shared Dr. Kyle Coffey and outlines the mechanical and metabolic changes seen with high intensity resistance training, BFR with low intensity resistance training, and low intensity resistance training alone.
My husband has been seeing a fantastic Physical Therapist who understood how much atrophy was impacting my husbands recovery and she recommended we start using BFR to augment his recovery. We started out at home with an occlusion wrap but soon realized that an BFR cuff would be a more controlled approach. With the wrap alone, my husband struggled to regulate the amount of pressure applied when wrapping his leg, he couldn’t complete a full set of exercises before his leg was too fatigued and he asked if it was ok that his toes were going numb. I told him not to wrap it up that tight, but he commented that it was “hard to get it right”.
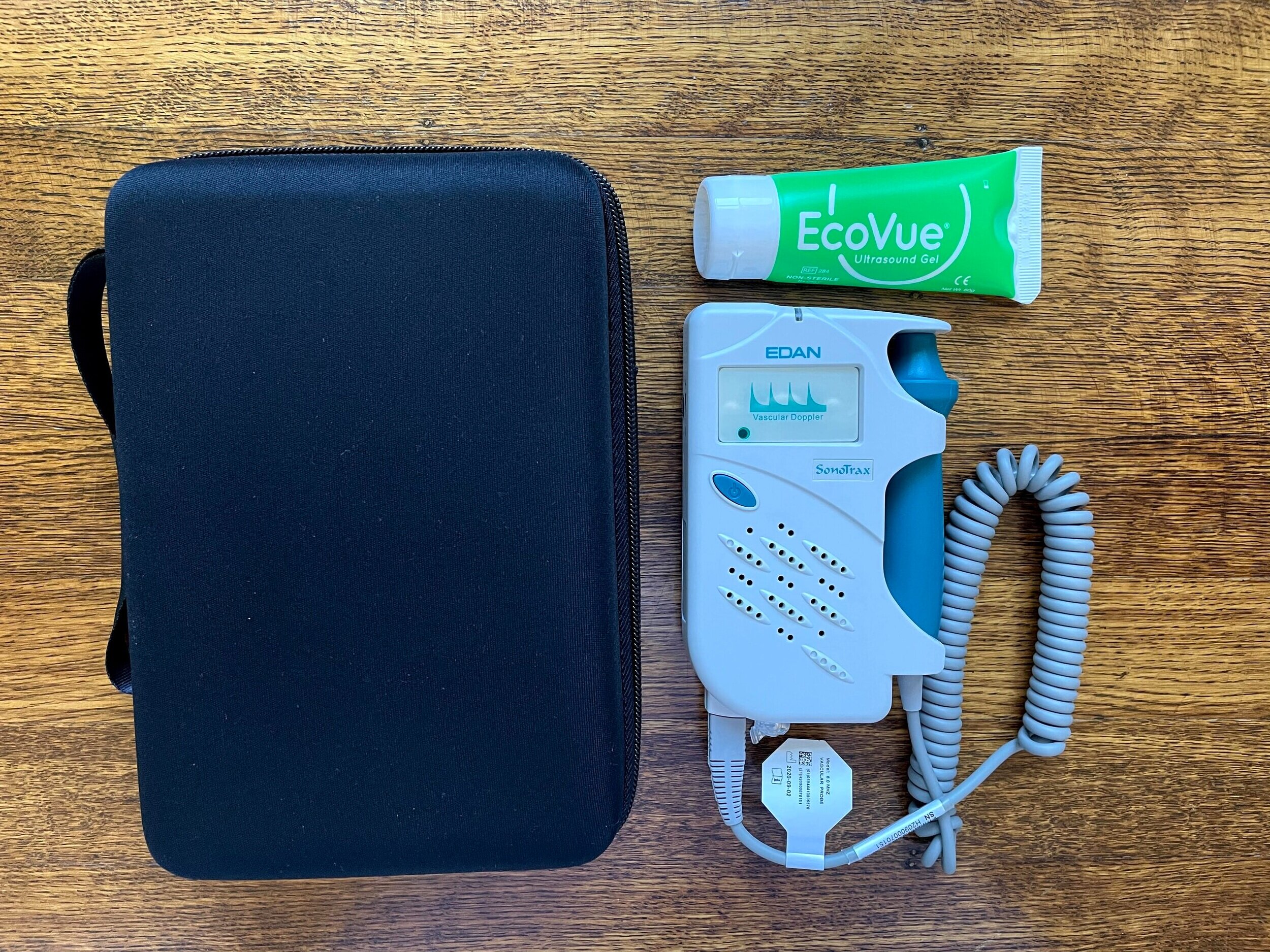
Intrigued, I took an online certification, bought a doppler US and cuffs for the upper and lower limb and so we could continue his rehabilitation at home. Following this course, I was able to understand how to individualize occlusion pressures for each limb, appreciate how important exercise selection and dosage was and confidently adapt load to ensure that enough exercises could be performed to create the metabolic stress described above. It was great to learn that there is a consistent protocol to follow when creating a treatment plan (Scott, et al., 2015).
Limb occlusion pressure for the upper limb is 30-50%, for the lower limb is 60-80%. This should be measured each session.
Once inflated, the cuff remains inflated for the entire duration of the set. Rather than deflating them to continue exercising, you should alter the exercise load to continue movement. After each exercise is complete, you can deflate the cuff for a break before moving onto the next exercise.
For strength/hypertrophy of the lower limb the desired intensity is 10-30% 1RM. Therefore a thorough strength assessment is required to determine the correct starting point.
The goal is 4 sets with 30 repetitions in the first set, then the remaining 3 are each 15 repetitions.
Rest 30-60 seconds between each set and no longer (otherwise this changes the lactate accumulation in the muscle).
The full program will take around 6-10 minutes to complete.
Allow for 3-5 minutes of re-perfusion post BFR.
Complete 2-3 times a week.
Completing BFR at home under the guidance of his therapist allowed me to explore how BFR felt from the patient’s perspective. I was interested in understanding how much time does it add to home programs, how comfortable is it, what does it feel like the following day etc.
What I learnt is that you really do need two people to measure individual occlusion pressure each session and this adds time to your program. There were times when I would find my husband doing BFR by himself and I asked how he measured the cuff pressure and he replied he could “feel” the right pressure and after multiple sessions he surprising actually got quite accurate in his guessing. I’m sure your patients are probably going to give it a crack as well, so make sure you educate them on how to use it safely.
We also learnt that each limb had a different tolerance to exercise and occlusion pressure (due to differences in muscle mass, circumference, and adipose tissue) and therefore a different treatment plan was needed for each lower limb. Compared to exercise without cuffs, the cuffs are slightly more uncomfortable, but they do not interrupt the exercises/movements. With BFR, we were able to achieve fatigue with exercises such as the active straight leg raise or isometric quad sets which matched his initial strength level and there was no discomfort reported the following day. This meant my husband could increase the frequency of rehabilitation sessions to increase muscle strength and size. After 4 weeks there was a considerable change in his strength and muscle bulk that allowed him to complete bilateral strengthening exercises with more even loading between legs. It felt like a game changer and the kick starter that was missing all along.
BFR in ACL rehab
Quadricep muscle strengthening post ACL reconstruction is incredibly important for successful return to sport and function. It makes sense then, that researchers are eager to understand if BFR can augment the healing process and accelerate the return of strength without risking overload of the healing graft and tissues. A few systematic reviews have been published in the past 2-3 years researching this topic. Many of them only have 3-4 high quality papers to evaluate, which is not very big. Even though this research is only in its infancy, many papers are publishing positive outcomes.
A systematic review in 2021 included four studies exploring the impact of BFR on muscle CSA and strength post ACLR (Bobes Álvarez, et al., 2021). When looking more closely at the included studies, they all followed a different strength and BFR protocol. Each had some aspects of the protocol listed about such as %1RM, dosage of sets, but none of them follow all the same protocol elements. It is therefore it is challenging to draw strong conclusions about the validity of the results founds.
Another systematic review I dug into explored three RCTs which all examined different aspects of BFR in early post-op recovery (Lipker, et al., 2019). One looked at BFR in conjunction with an exercise protocol with a standard cuff pressure of 180mmhg. The second looked at BFR without exercise using the 5 min inflation 3-minute deflation protocol. The third looked at BFR with the leg immobilized. Again, it’s important to read more deeply into the details because what we see here is that none of these studies followed the same protocol that I learnt about in the course. And none are individualized to the patient.
I did come across one great study during my search. In 2019, Hughes, et al., published a fantastic RCT from the UK. Their study included 28 ACLR with hamstring graft and evaluated strength gains following an eight-week training program. High resistance training was established at 70% 1RM and low resistance at 30% 1RM. Many of the other protocol metrics were the same as what I have learnt with regards to pressure and dosage. What they concluded is that BFR with LRT can improve muscle hypertrophy and strength similar to high resistance training but with greater reduction in knee joint pain and effusion. Overall there were greater improvements in physical function in the BFR group suggesting that BFR with LRT may be more appropriate in this patient population (Hughes, et al., 2019, p.1788). This is so exciting, that BFR can have an analgesic effect, combat disuse atrophy and assist with return to baseline strength.
I want to emphasize that the research growing around BFR is far more widespread that the post-operative population. Researchers are looking at its impact on aerobic capacity, bone density, cardiovascular implications, high level performance, platelet count and more. This blog is more a reflective piece on the starting point for my learning around BFR.
Online certification
Curious to know more about BFR I started looking at online training options that covered EBP specific to physiotherapy. I chose to study the online certification program hosted through The Modern Manual Therapist and created by Dr. Kyle Coffey. It’s a full 1-day online workshop that you can complete at your one pace from home. You receive pdf lecture slides, print-out slides of key summary material, and plenty of videos including doppler US and BP. It is incredibly well researched, yet only presents the content which is clinically applicable and was a worthwhile investment of my time.
This BFR workshop present by Dr. Coffey begins with an excellent overview of exercise physiology and how it relates to BFR specifically. He takes the time to educate his audience about understanding physiology and appreciating the importance of knowing what physiological adaptations we are trying to achieve with this form of treatment. He talks about why vital signs are important to measure and how pharmacology impacts BFR prescription. There is a video dedicated to patient safety, patient selection, and contraindications to BFR.
The topic of strength assessment is also covered in detail including; measuring limb circumference and understanding how we can use multiple repetition max (MRM) to predict 1RM. This is particularly valuable since patients who may be seeking strength gains have tissue pathologies/injuries that make measuring a 1RM unsuitable at the beginning of treatment. Early measurement of strength is one of the most important elements that will drive this approach. He explains why dosage and exercise prescription is the key to success with BFR and what the research shows us about implementing BFR protocols in a patient-centered manner.
Conclusion
When I first heard about BFR I was despondent. “Not another treatment technique” were my exact thoughts. But then I learnt about what BFR is trying to achieve and I realized that I could use this with so many of my patients, but firstly, on my husband. The concept that we can create changes in hypertrophy, muscle cross sectional area, aerobic capacity and even bone density with low load training to augment the healing process, to speed up recovery, to accelerate return of function, that is what BFR is driving forward. It is so exciting. We don’t have to wait for pain or ROM or tissue loading to improvement before embarking on a strengthening program. With the correct patient selection, the right exercise prescription and careful individual assessment – we can safely begin strength training with low load exercises that wouldn’t typically result in strength gains.
Personally, I thought it was so positive to read several blogs, watch videos, take the Medbridge and The Modern Manual Therapist courses and read many original papers to come to the same conclusion, to see authors sharing the same information and the same message. Consistency in content is what will make our implementation of the treatment technique successful. It was wonderful to find such high-quality material accessible online and I hope this blog inspires you to look into BFR further if you haven’t yet already.
Sian
References
Baron, J. E., Parker, E. A., Duchman, K. R., & Westermann, R. W. (2020). Perioperative and Postoperative Factors Influence Quadriceps Atrophy and Strength After ACL Reconstruction: A Systematic Review. Orthopaedic Journal of Sports Medicine, 8(6), 2325967120930296.
Brandner, C. R., Clarkson, M. J., Kidgell, D. J., & Warmington, S. A. (2019). Muscular adaptations to whole body blood flow restriction training and detraining. Frontiers in physiology, 10, 1099.
Bobes Álvarez, C., Issa-Khozouz Santamaría, P., Fernández-Matías, R., Pecos-Martín, D., Achalandabaso-Ochoa, A., Fernández-Carnero, S., ... & Gallego-Izquierdo, T. (2021). Comparison of Blood Flow Restriction Training versus Non-Occlusive Training in Patients with Anterior Cruciate Ligament Reconstruction or Knee Osteoarthritis: A Systematic Review. Journal of Clinical Medicine, 10(1), 68.
Charles, D., White, R., Reyes, C., & Palmer, D. (2020). A SYSTEMATIC REVIEW OF THE EFFECTS OF BLOOD FLOW RESTRICTION TRAINING ON QUADRICEPS MUSCLE ATROPHY AND CIRCUMFERENCE POST ACL RECONSTRUCTION. International Journal of Sports Physical Therapy, 15(6), 882.
Hughes, L., Rosenblatt, B., Haddad, F., Gissane, C., McCarthy, D., Clarke, T., ... & Patterson, S. D. (2019). Comparing the effectiveness of blood flow restriction and traditional heavy load resistance training in the post-surgery rehabilitation of anterior cruciate ligament reconstruction patients: a UK National Health Service randomised controlled trial. Sports Medicine, 49(11), 1787-1805.
Ilett, M. J., Rantalainen, T., Keske, M. A., May, A. K., & Warmington, S. A. (2019). The effects of restriction pressures on the acute responses to blood flow restriction exercise. Frontiers in physiology, 10, 1018.
Kilgas, M. A., Lytle, L. L., Drum, S. N., & Elmer, S. J. (2019). Exercise with blood flow restriction to improve quadriceps function long after ACL reconstruction. International journal of sports medicine, 40(10), 650-656.
Loenneke, J. P., Abe, T., Wilson, J. M., Ugrinowitsch, C., & Bemben, M. G. (2012). Blood flow restriction: how does it work?. Frontiers in physiology, 3, 392.
Lipker, L. A., Persinger, C. R., Michalko, B. S., & Durall, C. J. (2019). Blood flow restriction therapy versus standard care for reducing quadriceps atrophy after anterior cruciate ligament reconstruction. Journal of sport rehabilitation, 28(8), 897-901.
Lu, Y., Patel, B. H., Kym, C., Nwachukwu, B. U., Beletksy, A., Forsythe, B., & Chahla, J. (2020). Perioperative blood flow restriction rehabilitation in patients undergoing ACL reconstruction: a systematic review. Orthopaedic journal of sports medicine, 8(3), 2325967120906822.
Patterson, S. D., Hughes, L., Warmington, S., Burr, J., Scott, B. R., Owens, J., ... & Loenneke, J. (2019). Blood flow restriction exercise: considerations of methodology, application, and safety. Frontiers in physiology, 10, 533.
Scott, B. R., Loenneke, J. P., Slattery, K. M., & Dascombe, B. J. (2015). Exercise with blood flow restriction: an updated evidence-based approach for enhanced muscular development. Sports medicine, 45(3), 313-325.
Online training
The Manual Therapist
BFR cuffs and Doppler US equipment
I purchase my cuffs and Doppler US from Modern Manual Therapist and have been extremely happy with the quality and comfort of the equipment.
ACL Masterclass
https://www.learn.physio/courses
Medbridge
First, I watched three Medbridge videos which took 3-4 hours to complete and sparked my curiosity around the physiological changes that occur during BFR which lead to these adaptations in muscle hypertrophy and cross sectional area. To access these videos you need a Medbridge subscription.
Blogs
https://thebarbellphysio.com/science-blood-flow-restriction-training/
https://www.bodybuilding.com/content/your-complete-guide-to-blood-flow-restriction-training.html
https://theprehabguys.com/blood-flow-restriction-training-in-a-nutshell/
https://www.physio-pedia.com/Blood_Flow_Restriction_Training